This is an automatically translated article.
Posted by Doctor CKII Nguyen Thi Hoai Nam - Department of Surgical Anesthesia - Vinmec Central Park International General Hospital
1. Explain the concept of sedation, regional anesthesia
Sedation is a condition in which the patient's awareness of the surrounding environment is reduced and their response to external stimuli is reduced under the influence of drugs. Depending on the dose of drug used, sedation can be divided into 4 levels from mild to deep, including: mild sedation, moderate sedation, deep sedation and general anesthesia.
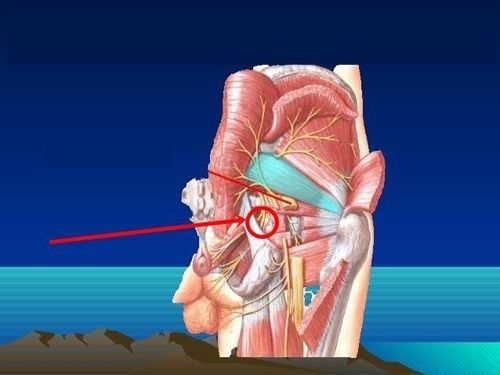
Regional anesthesia, also known as regional anesthesia, is a method of temporarily losing or reducing sensation in a part or area of the body, but without losing consciousness, the patient remains awake. Regional anesthesia includes neuraxial anesthesia (spinal anesthesia, epidural anesthesia) and peripheral nerve anesthesia (plexus anesthesia, nerve trunk anesthesia, muscle fascia...).
Regional anesthesia is currently a trend in multimodal analgesia for postoperative pain management. The combination of regional anesthesia with common analgesics reduces the use of Morphine after surgery, so it can reduce the side effects of the drug such as itching, vomiting, nausea, urinary retention, respiratory depression, addiction, increased pain, and progressive pain. develop chronic pain after surgery...

Gây tê vùng trong điều trị răng miệng
2. Advantages of regional anesthesia
Regional anesthesia offers advantages such as:
Postoperative pain relief and better recovery Reduce the dose of Morphine Reduce the length of hospital stay Reduce the rate of re-hospitalization Reduce the rate of vomiting and nausea after surgery Patients can be active soon after surgery and participate in physical therapy early Increase satisfaction rate, improve patient's quality of life Besides, regional anesthesia still has some unwanted side effects including anesthetic poisoning (LAST) and injury to patients. nerve injury. The question is whether sedation during regional anesthesia can help avoid these complications?
3. Why should regional anesthesia be performed in patients under general anesthesia or sedation?
Some believe that when the patient is under general anesthesia or deep sedation, it will be beneficial to perform regional anesthesia because:
Increases the safety of anesthesia by reducing the patient's sudden movement that can stabbing needles into vital body structures. Increases the number of patients who agree to have anesthesia because most of them are afraid of injection while awake. This will increase the number of patients who benefit from regional anesthesia for surgery or pain relief.

Gây tê vùng giúp giảm cử động đột ngột của người bệnh trong phẫu thuật
4. Why should regional anesthesia be performed in patients who are awake or lightly sedated?
On the contrary, there is a perception that the patient should be awake or only slightly sedated during anesthesia, which will help to recognize early signs of poisoning because:
Patients who are awake or only slightly sedated can feel and notify the doctor. early warning signs of anesthetic toxicity before a toxic dose is administered. Pain and paresthesias, which are indicative of nerve damage, can be recognized and reported to the physician when a needle is inserted into a nerve structure. Many studies have been carried out to demonstrate the advantages and disadvantages of regional anesthesia with or without sedation or anesthesia.
5. Does deep sedation or anesthesia affect the patient's ability to recognize and report symptoms?
For local anesthetic poisoning: In a study by the Department of Anesthesiology at Virginia Mason Medical Center and the University of Washington, sedation with Midazolam and Fentanyl reduced the reliability of the Lidocaine test for regional anesthesia. Therefore, it is recommended to use Epinephrine as a test drug. Patients who report symptoms of CNS toxicity are not 100% sensitive because young children, the elderly, have language barriers, so the symptoms are not sensitive enough or incomplete. If local anesthetic is mistakenly injected into a rapid blood vessel, the patient may have a seizure before they are aware and report CNS symptoms. The American Society of Regional Anesthesiology and Anesthesia recommends: The ability of anesthesia or deep sedation to mask early symptoms of local anesthetic toxicity is not a valid reason to forego regional and epidural anesthesia. stiffness under anesthesia or deep sedation.

Người bệnh có thể bị tai biến ngộ độc thuốc tê
An thần sâu có thể dẫn tới tổn thương thần kinh ở cả người lớn và trẻ em
Sedation while performing anesthesia for the benefit or harm area still has no exact answer. Studies that provide only recommendations for practice include:
There are no guidelines to demonstrate that local anesthesia or deep sedation reduces the risk of local anesthetic toxicity and neurologic complications In humans Regional anesthesia should not be routinely performed under general anesthesia or sedation. In children, regional anesthesia under general anesthesia or deep sedation may be appropriate. Stepwise intermuscular anaesthesia should not be administered to children under general anesthesia or sedation. The risk-benefit ratio should be weighed before making a decision. At Vinmec Health System, patients are always assessed before surgery according to the pre-anesthesia examination process to have an appropriate anesthetic and anesthetic plan. The modern monitor system fully monitors vital signs during and after surgery to help detect the patient's abnormalities early in order to promptly handle possible complications. Developing regional anesthesia under ultrasound guidance is Vinmec's strength, helping patients to reduce pain well and safely during and after surgery.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE.
SEE MORE
Is cesarean delivery painful? Spinal anesthesia for caesarean section Differentiate between epidural and spinal anesthesia