This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Autoimmune pancreatitis and immunoglobulin G4-associated disease (IgG4-RD) are new disease entities characterized by an enhanced IgG4 antibody response. Serum levels of IgG4 antibodies are widely used as a useful biomarker for diagnosis and monitoring of disease activity in autoimmune pancreatitis and IgG4-RD.
1. Overview
Immune-system alone disorders, formerly known as autoimmune pancreatitis (AIP), autoimmune cholangitis, and autoimmune sclerosing cholangitis, are now considered to be specific disease-associated manifestations. systemic immunoglobulin G4 (IgG4-RD). New biomarkers need to be identified based on an understanding of the pathophysiology of autoimmune pancreatitis and IgG4-RD. Recently, the authors found that the activation of plasmacytoid dendritic cells that produce both interferon-α (IFN-α) and interleukin-33 (IL-33) mediates autoimmune pancreatitis in mice as well as murine autoimmune pancreatitis. related to human G4 systemic immunoglobulin. Autoimmune pancreatitis and immunoglobulin G4-associated disease (IgG4-RD) are new disease entities characterized by an enhanced IgG4 antibody response. Serum levels of IgG4 antibodies are widely used as a useful biomarker for diagnosis and monitoring of disease activity in autoimmune pancreatitis and IgG4-RD. Recent studies have emphasized the importance of cytokine as well as chemokinetic responses in the immunogenicity of these disorders.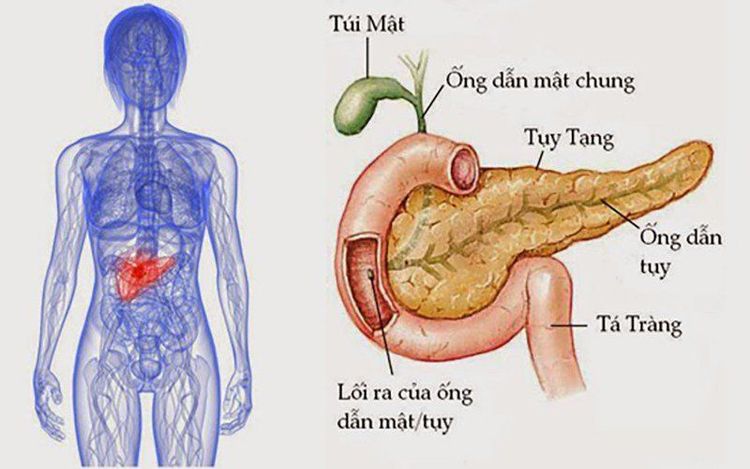
2. Role of the innate immune response in autoimmune pancreatitis
It remains uncertain whether innate immune responses are shared by peripheral blood and affected organs in autoimmune pancreatitis as well as by IgG4-RD. To identify the innate immune cells responsible for the development of autoimmune pancreatitis and IgG4-RD, the authors used an experimental mouse model of autoimmune pancreatitis and IgG4-RD. Repeated intraperitoneal injections of polyinosinic-polycytidylic acid [poly(I:C)] into MRL/MpJ mice resulted in the development of autoimmune pancreatitis characterized by destruction of pancreatic duct structures, invasion immune cell entry and fibrosis. Therefore, an experimental mouse model of autoimmune pancreatitis recapitulates the pathological findings observed in human autoimmune pancreatitis.
3. Role of storiform fibrosis in autoimmune pancreatitis Although storiform fibrosis is one of the signature findings in human autoimmune pancreatitis, molecular mechanisms account for its induction and generation. This fibrotic response is still not well understood. Recently, the authors discovered that the type I IFN-IL-33 axis plays a proinflammatory and pro-fibrogenic role in chronic alcoholic pancreatitis. The production of type I IFNs by pancreatic cells works together with TNF-a produced from pancreatic phage macrophages to potently induce IL-33 by squamous cells. With pDC-induced type I IFN mediating experimental autoimmune pancreatitis, the authors hypothesized that IL-33 is involved in the induction of chronic fibroinflammatory responses in the pancreas. pDCs accumulate in the pancreas after multiple injections of poly(I:C), inducing IL-33 in a type I IFN-dependent manner. Importantly, the blockade of IL-33-mediated signaling pathways by a Ab acts against the IL-33 receptor, thereby attenuating the chronic inflammatory responses of the pancreas, which is accompanied by a marked reduction in pro-fibrinolytic cytokines such as IL-13 and TGF-β1.
4. Role of IFN-α and IL-33 Factors Immunofluorescence studies of pancreatic specimens from patients with autoimmune pancreatitis and IgG4-RD confirmed pancreatic localization of pDCs. IL-33 expression. Taken together, these results support the idea that activation of pDCs followed by production of IFN-α and IL-33 mediates both experimental and human autoimmune pancreatitis. It should be noted, however, that pDC is not the sole cellular source of IL-33. For example, M2 macrophages have been shown to colocalize with IL-33 in the salivary glands of IgG4-RD patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Hara A, Watanabe T, Minaga K, Yoshikawa T, Kamata K, Kudo M. Biomarkers in autoimmune pancreatitis and immunoglobulin G4-related disease. World J Gastroenterol 2021; 27(19): 2257-2269 [DOI: 10.3748/wjg.v27.i19.2257]