This is an automatically translated article.
In case the patient has a blood clotting disorder, a normal person who has a caesarean section is also likely to have some blood clots, tissue cells, fat, air bubbles... entering the blood stream to the lungs and causing a condition. postpartum pulmonary embolism. If not treated promptly, it can endanger the mother's life.
1. What is pulmonary embolism?
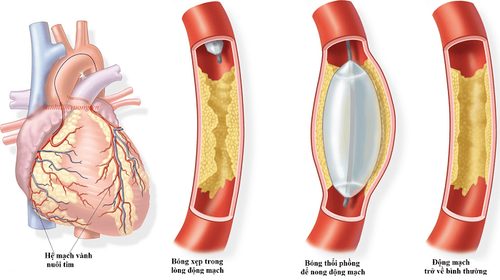
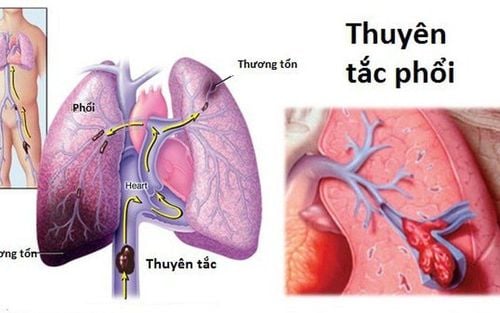
Pulmonary embolism is a blockage in the blood vessels of the lungs caused by blood clots. Pulmonary embolism can occur in the central artery of the lung or near the edge of the lung. In the case of large blood clots causing obstruction near the center of the lung, severe symptoms will occur in the patient and called a major pulmonary embolism, which can be life-threatening.
The majority of patients with pulmonary embolism are caused by deep vein thrombosis. Therefore, people at high risk of pulmonary embolism are those who are prone to deep vein thrombosis, some other risk factors are patients who are immobile for a long time, have serious medical conditions, and major surgery.
Postpartum pulmonary embolism can also be caused by obstructions, amniotic fluid due to pregnancy complications, air when placing a central venous catheter into the blood, tissue, fat, and air bubbles.. .enters the bloodstream and then travels to the lungs during caesarean section. The risk of postpartum pulmonary embolism can be significantly reduced if the mother is mobilized early or, for special populations, is given antithrombotic drugs.
Bệnh lý thuyên tắc phổi là tình trạng tắc nghẽn tại mạch máu của phổi do các cục máu đông gây ra
2. What is the cause of postpartum pulmonary embolism?
According to specialists, the main cause in most cases of postpartum pulmonary embolism is a blood clot that has formed in a deep vein, also known as a venous thrombosis, a blood clot. This clot travels through the bloodstream and becomes trapped in one of the blood vessels in the lungs.
In some other rarer cases, postpartum pulmonary embolism is not caused by blood clots, but by other factors such as:
Amniotic fluid during pregnancy or during delivery – amniotic fluid embolism (amniotic fluid embolism) rare) Large air bubbles in the vein (rare) Fat drops from the marrow of a broken bone Foreign body from a syringe that is not as clean as a syringe for injecting drugs A small piece of tumor has broken off from a large tumor in the body as in cancer.
3. Risk of pulmonary embolism in pregnant and postpartum women
The risk of pulmonary embolism during pregnancy is 5 times that of normal women and 2 times after giving birth. Venous thrombosis usually forms in the deep vein on the left leg. As you approach the stage of childbirth, many changes occur that increase the blood's ability to clot to limit blood loss during pregnancy and delivery.
In addition, at the time of delivery, the strong contractions during labor also have a strong impact on the veins in the pelvis and cause minor damage to the veins, increasing the risk of developing a clot. postpartum haemorrhage and pulmonary embolism.
The risk of pulmonary embolism during pregnancy is increased if the woman:
Plans to have a cesarean section Are overweight High blood pressure Have pre-eclampsia Have a genetic predisposition to thromboembolic disease Have a close relative or family history of the disease Venous thromboembolism or blood clotting disorder Pregnant women over 35 years of age Smoking Have varicose veins.
4. Symptoms of pulmonary embolism

Khi bị thuyên tắc phổi sau sinh, phụ nữ thường bị khó thở với mức độ thay đổi từ nhẹ đến rất nặng
Postpartum pulmonary embolism symptoms will depend on whether the site of the clot is large or small and how long the patient's lungs are strong enough to deal with the clot. Postpartum mothers or those with pre-existing medical conditions often have poor health, so symptoms will be more severe, including:
Postpartum dyspnea with varying degrees of mild to very severe pleuritic chest pain, sharp pain when giving birth inhaling The patient cannot take a deep breath, because the pain causes the person to hold his or her breath Coughing up blood Slight rise in temperature A rapid heartbeat Feeling weak, unwell, or dizzy. Patients with major pulmonary embolism can cause cardiac arrest and lead to rapid death despite immediate resuscitation. Some symptoms of deep vein thrombosis that patients may experience include: Sudden pain in the calf, swelling of one leg or foot, muscle pain in the calf muscle, hot and red calf, maybe bruises on the upper body. skin.
5. How is postpartum pulmonary embolism treated?
Women with postpartum pulmonary embolism can be spectacularly saved through early detection and intervention, some of the treatment methods include:
Anticoagulant therapy, usually started immediately when pulmonary embolism is suspected to prevent aggravation while waiting for test results. Anticoagulation therapy should be continued for up to 3 months after pulmonary embolism in most cases.
The patient will breathe oxygen in the initial stage to improve dyspnea and hypoxemia.
In some cases, the patient will receive intravenous fluids to support circulation and close monitoring and admission to the intensive care unit may be necessary if the patient is unwell or the pulmonary embolism is large.
Currently, at Vinmec International General Hospital, fibrinolysis is being applied for emergency treatment of patients with pulmonary embolism. With modern imaging equipment, CT perfusion results are available within 7 minutes and performed routinely. The technique is performed by a team of qualified, experienced doctors and modern equipment and professional services.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.