This is an automatically translated article.
The article was professionally consulted by MSc Vu Tan Phuc - Gastroenterologist - Department of Medical Examination & Internal Medicine, Vinmec Phu Quoc International General Hospital.Ulcerative colitis not only makes patients feel extremely uncomfortable but also greatly affects life, work and activities. There is currently no cure for this disease, the aim of treatments is to control the condition.
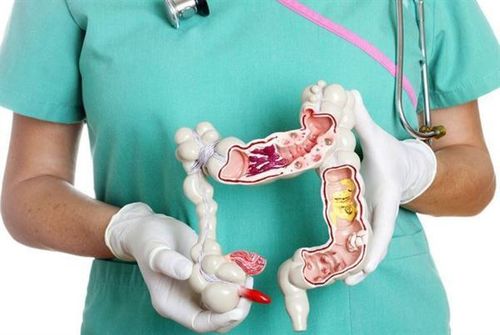
1. What is ulcerative colitis?
Ulcerative colitis (UC) is an inflammatory bowel disease that causes irritation, inflammation, and ulcers in the lining of the large intestine (also called the colon). Currently, there is no definitive treatment for this disease. However, existing treatments will help people control the disease.2. Causes of Ulcerative Colitis
The exact cause of ulcerative colitis is still unknown. In the past, it was suggested that diet and food were the main causes of ulcerative colitis, but it is only the factors that are more serious than the condition.Ulcerative colitis occurs when the immune system malfunctions. Normally, it attacks intruders, just like the common cold. When you have a stomach ulcer, the immune system thinks that food, intestinal bacteria and the cells lining the stomach are invaders that cause inflammation and ulcers.
Genetics is also a cause of ulcerative colitis because the disease is common in patients with a close relative with the disease.

3. Risk factors for ulcerative colitis
Several factors can put you at an increased risk of developing ulcerative colitis, including:Age: Ulcerative colitis usually occurs between the ages of 15 and 30, and some cases do not develop until: to 60 years of age Race: The risk of ulcerative colitis is highest among people of Ashkenazi Jewish descent. Family history: Your risk of developing ulcerative colitis may be up to 30% higher if you have a close relative with the condition. Food and psychological stress are not the cause of UC, but they do influence a wide range of symptoms.

4. Types of ulcerative colitis
Classification of ulcerative colitis is usually based on its location. Types of ulcerative colitis, including:Ulcerative colitis : Usually the mildest form, it affects only the rectum, part of the colon, limited to the area near the anus. Rectal bleeding may be the only sign of the disease. Proctosigmoid inflammation: Inflammation occurs in the rectum and sigmoid colon. Symptoms of the disease include bloody diarrhea, abdominal pain, your inability to move your bowels, despite the urge to do so (tenesmus). Left-sided colitis: Causes pain in the left side of the abdomen. Signs of the disease include bloody diarrhea, or possible weight loss despite eating normally. You will have inflammation from the rectum up through the left side of the colon. Colitis: Usually affects your entire colon. It can cause bouts of severe diarrhea, abdominal pain, pain, fatigue, and severe weight loss. Acute ulcerative colitis: This rare condition affects the entire colon and causes severe pain, severe diarrhea, bleeding, and fever.

5. Symptoms of ulcerative colitis
The main symptom of ulcerative colitis is bloody diarrhea, which may appear pus in your stool. Some other symptoms, including:Sudden pounding of pain Abdominal pain Not feeling hungry Weight loss Feeling tired Fever Dehydration Joint pain or aches Sores Pain when you try to see Anemia Going to the toilet at night Pain or bleeding when going to the toilet Symptoms can suddenly flare up, go away, and come back. You may not show any signs of the disease for many years. Other intestinal diseases can have some similar symptoms, such as Crohn's disease.
Ulcerative colitis affects only the large intestine and lining Crohn's disease causes inflammation, but it affects other sites in the digestive tract Irritable bowel syndrome has some of the same symptoms as UC, but it does not cause inflammation or ulceration. Instead, it's a problem with the organs in your gut.

6. Diagnosing ulcerative colitis
Several methods are commonly used to diagnose ulcerative colitis, including:Blood tests: Anemia or inflammation may be a sign that you have ulcerative colitis Stool samples: May help Your doctor rules out an infection or parasite in your colon. They can also show if there's blood in the stool that you can't see. Sigmoidoscopy: Allows the doctor to see the lower part of the colon by inserting a bendable instrument tube into the lower colon through the anus. Instrument tube with small light and camera. The doctor may also use an instrument to remove a portion of the lining of the lower colon for a biopsy. Colonoscopy: The procedure is similar to a sigmoidoscopy, only with a colonoscopy, your doctor can see your entire colon, not just the lower part. X-ray: This method is less common in the diagnosis of disease, but the doctor may order it in special cases.

7. Treatment of ulcerative colitis
Treatment for UC has two main goals, the first is to make you feel better and to minimize the effects of your symptoms. The second is to prevent the disease from progressing. You may need a combination of diet changes, medication, or surgery to achieve those goals.Diet: Certain foods can make symptoms worse. You will feel more comfortable eating soft, bland foods than spicy or high-fiber foods. If you cannot absorb the sugar in milk called lactose (meaning you are lactose intolerant), your doctor may ask you to stop eating dairy products. A balanced diet with plenty of fiber, lean protein, fruits and vegetables helps provide adequate vitamins and nutrients. Medications: Your doctor will prescribe several different medications, including: Antibiotics: Helps fight infections Aminosalicylate: 5-aminosalicylic acid (5-ASA) found in this medicine helps fight inflammation and control symptoms. Corticosteroids: If aminosalicylates don't work or your symptoms become increasingly severe, your doctor may prescribe you to take them for a short time. Colon. It takes a while for the medicine to take effect. You may not notice any changes for up to 3 months. Biologic drugs: These are made from proteins in living cells instead of chemicals. Biologics are used for people with severe ulcerative colitis. Loperamide: Helps slow or stop diarrhea. Consult your doctor before taking Surgery: If other treatments don't work or the UC becomes severe, you may need surgery to remove your colon and rectum. If an ileostomy is performed, your doctor can make a small pouch out of your small intestine and attach it to the anus. This technique, called ileal pouch anastomosis (IPAA), allows your body to flush out waste products normally, so you don't need to wear a bag.

8. Complications of ulcerative colitis
Complications of ulcerative colitis can include:Bleeding: This can lead to anemia Osteoporosis: Your bones may become weak due to diet or if you take a lot of corticosteroids Dehydration: You You may need intravenous fluids (intravenous or IV) if the large intestine cannot absorb enough. Inflammation: This can affect joints, skin, or eyes. Fulminant colitis: If UC is severe, your colon may rupture, or the infection may spread in your body. Your intestines will stop moving waste, and your abdomen will swell. Liver disease: The bile ducts or liver may become inflamed Colon cancer: Ulcerative colitis puts you at higher risk of colon cancer, especially if the entire large intestine is affected or if you have UC in a long time. Most ulcerative colitis is a chronic or long-term condition. Some will show symptoms of the disease, others may not see any symptoms. About 10% of people with UC are impacted by the disease's symptoms at first, and the condition rapidly worsens, with serious complications. In some cases, the disease spreads to the large intestine over time. This carries a risk of colon cancer, but about half of them have a chance of survival if doctors find the disease early and remove the colon.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: webmd.com