This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International HospitalSince entering the market, proton pump inhibitors (PPIs) have revolutionized the treatment of gastroesophageal reflux disease (GERD) and become the most powerful class of drugs for the treatment of this disease. In today's article, we will discuss treatment-resistant reflux esophagitis, the definition of its clinical features, and the treatment response to PPIs.
1.Nonerosive Reflux Disease (NERD) Studies have demonstrated that up to 70% of patients with typical symptoms of GERD, in primary care, have NERD. Therefore, NERD is considered the most common presenting form of GERD.
Several studies evaluated the effectiveness of PPIs in patients with NERD. In a double-blind, randomized, multicenter study, omeprazole 20 mg once daily was compared with placebo in the control of symptoms in 209 NERD patients. After 4 weeks of treatment, 57% of patients in the omeprazole group had no heartburn, 75% had no acid reflux, and 43% were completely symptom-free. In another study, NERD patients were randomized to omeprazole 20 mg/day; omeprazole 10mg/day; or placebo. The study authors found that at week 4, 46% of patients treated with omeprazole 20 mg/day, 31% treated with omeprazole 10 mg/day, and 13% of those treated with placebo reported relieve heartburn completely. Miners et al enrolled 203 patients with NERD who were randomized to rabeprazole 20 mg once daily or placebo. After 4 weeks, only 56.7% of patients receiving rabeprazole reported a significant reduction in symptoms compared with 32.2% of patients receiving placebo (P < 0.008).
Overall, the proportion of NERD patients who respond to standard doses of PPIs is approximately 20-30% lower than what has been observed in patients with erosive esophagitis. In a systematic review of the literature, the composite PPI symptom response rate was 36.7 (95% CI: 34.1–39.3) in patients with NERD and 55.5 (95% CI: 51). ,5–59,5) in people with erosive esophagitis. Therapeutic efficacy was 27.5% in NERD compared with 48.9% in erosive esophagitis. Furthermore, NERD patients demonstrate a direct relationship between response to PPI therapy and esophageal acid exposure. The more distal esophageal acid exposure, the higher the proportion of NERD patients reporting symptom resolution. This is in contrast to what has been observed in patients with erosive esophagitis, where the greater the esophagitis, the lower the response rate to once-daily PPIs. NERD patients also showed a later time to maintain symptom response when compared with patients with erosive esophagitis (two- to three-fold).

Studies have shown that approximately 30-50% of NERD patients show esophageal acid exposure in the physiological range. Patients with NERD and an abnormal pH test showed a 55% overlap of the total time of pH <4 when compared with those with erosive esophagitis and 50% when compared with those with Barrett's esophagus. Furthermore, the response to once-daily PPIs of NERD patients with an abnormal pH test appears to be similar to the response rates of patients with erosive esophagitis (75–85%).
Patients with NERD and a normal pH test are termed functional heartburn, defined as “episodic retrosternal burning in the absence of pathologic GER, disease-based movement disorder or resolution love the structure”. The functional heartburn group is divided into two subgroups. The first group included patients with a strong temporal relationship between heartburn symptoms and acid reflux events, regardless of the physiological level of acid exposure in the esophagus. This subgroup accounts for up to 40% of patients with functional heartburn and is referred to as esophageal hypersensitivity. Patients with esophageal hypersensitivity have a partial response to PPI therapy. In contrast, the remaining subgroup did not show any correlation between heartburn episodes and acid reflux events. These patients were unlikely to respond to any antireflux interventions. Factors other than acid reflux are likely to cause these patients' symptoms.
Patients with functional heartburn had the lowest rate of symptom response to once-daily PPIs when compared with other NERD patients. Lind et al showed that only 45% of patients with functional heartburn reported a sufficient reduction in heartburn symptoms when compared with other NERD patients. Thus, the functional heartburn group may have caused the low response rates of NERD patients to once-daily PPIs compared with patients with erosive esophagitis. Patients with functional heartburn were also responsible for the lack of difference in symptom response rates between NERD patients receiving the standard half-dose PPI once daily and those receiving the standard full-dose PPI once daily. everyday. It is recognized that NERD is the most common manifestation of GERD, affecting 70% of GERD patients in the community, and of these, up to 50% are functional heartburn patients, who have the lowest response rates. with PPIs once daily, one might then conclude that many patients with PPI failure originate in the NERD group, mainly the functional heartburn group.
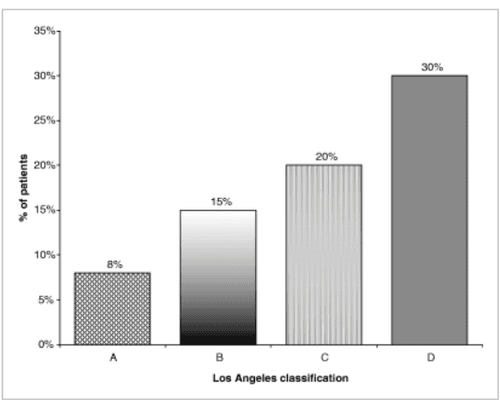
2. Erosive esophagitis Studies in patients with erosive esophagitis who were treated with PPIs once daily showed a cure rate of 88–96% after 8 weeks of treatment, regardless of label of PPIs used and baseline severity of erosive esophagitis. As a result, only 4–12% of patients with erosive esophagitis did not take PPIs once daily. As expected, patients with more severe esophagitis had a higher PPI failure rate than less severe patients. In a study that included 1284 patients with erosive esophagitis treated with two different PPIs once daily, 10.6–11.8% of those with grade 2 esophagitis did not heal after 4 weeks of treatment. treatment, compared with 26.5–30.2% in those with grades 3 and 4. Richter et al demonstrated that the failure rate of patients with erosive esophagitis received omeprazole 20 mg x 1 times/day or esomeprazole 40 mg once/day were 9.6% and 6.6% for Los Angeles class A; 28.7% and 10.6% for class B; 29.6% and 12.8% for block C; and 36.2% and 20% for grade D. (Figure 2).
Although PPIs are also very effective in reducing symptoms in patients with erosive esophagitis, there is a 10-15% difference between symptom resolution and mucosal healing.
Knowing that erosive esophagitis affects approximately 30% of GERD patients and most subjects with mild to moderate erosive esophagitis it is unlikely that patients with erosive esophagitis contribute to most of the failures. PPI once per day.
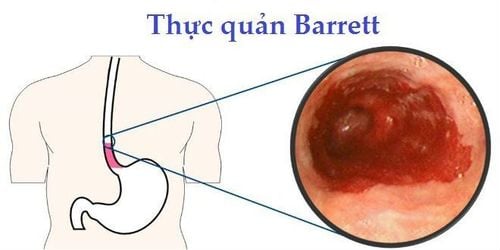
3. Barrett's esophagus (BE) The prevalence of Barrett's esophagus is 6-12% of all patients presenting to endoscopy with GERD-related symptoms, and 0.25–3.9% of patients with GERD. Unselected cases underwent upper endoscopy. According to one group, patients with Barrett's esophagus demonstrated the highest levels of acid exposure in the distal esophagus when compared with those with NERD or erosive esophagitis, indicating the need for aggressive anti-reflux therapy. more extreme. Furthermore, there is a strong correlation between the length of Barrett's esophagus and the degree of exposure to esophageal acid. Although the rate of symptom relief in patients with Barrett's esophagus treated with PPIs is 80%, there is a difference between symptom resolution and acid control in these patients. It has been shown that 20–40% of patients with Barrett's esophagus, whose symptoms resolved during PPI therapy, remain exposed to abnormal esophageal acid, by monitoring esophageal pH for 24 h. This phenomenon has been described even with high dose PPIs (up to four times daily) and does not appear to be dependent on patient resolution of symptoms. Katzka and Castell showed that of five Barrett's esophagus (BE) patients who received omeprazole daily (20–60 mg) and reported complete resolution of symptoms, four (80%) continued to be exposed to Abnormal esophageal acid. Similarly, Fass et al demonstrated that of the 25 BE patients receiving omeprazole 40 mg twice daily, almost a quarter remained exposed to abnormal acid and of these 67% were asymptomatic. In clinical practice, physicians will target symptom resolution in patients with BE, which may not be sufficient to control esophageal acid exposure in a significant minority. It is unclear whether continued abnormal acid exposure in patients with Barrett's esophagus on high-dose PPIs should be further therapeutically addressed. To date, there is no clear evidence that increasing the dose of PPIs is necessary in this situation. There are currently no data supporting a survival benefit with acid-reducing therapy, and there is no consensus on whether the endpoint of treatment in patients with Barrett's esophagus should be for complete acid control. Although, recent data suggest that PPI therapy can suppress tumor progression over time, significant regression of Barrett mucosal length has not been demonstrated. However, based on the current literature, it seems prudent to define PPI failure in patients with Barrett's esophagus who do not have adequate symptomatic relief and complete healing of associated esophagitis while taking this medication. PPIs once a day.
The phenomenon of PPI failure in patients with Barrett's esophagus has hardly been studied. Unfortunately, many studies have used high doses of PPIs in these patients as the initial treatment strategy. In one study, all BE patients receiving omeprazole 20 mg once daily were symptom-free. However, several studies using high-dose PPIs (omeprazole 80 mg, lansoprazole 60 mg, and omeprazole 60 mg once daily) demonstrated complete resolution of heartburn in 80–85% of patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
F. Fass , M. Shapiro , Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease – where next? Alimentary Pharmacology and Theurapeutics, Volume22, Issue2, July 2005 Vaezi MF. ‘Refractory GERD’: acid, nonacid, or not GERD? Am J Gastroenterol 2004; 99: 989– 90. Richter JE, Bochenek W. Oral pantoprazole for erosive esophagitis: a placebo-controlled randomized clinical trial. Pantoprazole US GERD Study Group. Am J Gastroenterol 2000; 95: 3071– 80.