This is an automatically translated article.
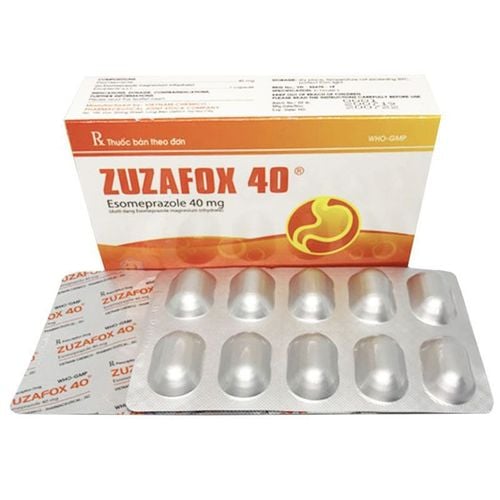
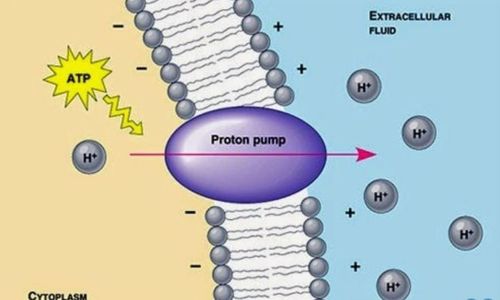
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International HospitalSince entering the market, proton pump inhibitors (PPIs) have revolutionized the treatment of gastroesophageal reflux disease (GERD) and become the most powerful class of drugs for the treatment of this disease. In today's article, we will discuss treatment-resistant reflux esophagitis, the definition of its clinical features, and the treatment response to PPIs.
Failure of PPI proton pump inhibitors has become a common clinical dilemma common in gastroenterology clinics and increasingly encountered in medical settings. The underlying mechanisms are varied and may overlap. Most patients with proton pump inhibitor failure likely stem from a non-erosive reflux disease phenotype. Currently, available diagnostic modalities provide limited clues to the underlying etiology of this poorly defined pathology. Treatment is mainly based on increasing the dose of proton pump inhibitors. However, new insights into the pathophysiology of proton pump inhibitor failure have the potential to provide alternative treatment options.
1.Overview of the failure of antacids in the treatment of reflux esophagitis Since their introduction on the market nearly two decades ago, proton pump inhibitors (PPIs) have created a sensation. revolution in the treatment of gastroesophageal reflux disease (GERD). Significant progress has been made in symptom resolution and healing of the esophageal mucosa that has positioned PPIs as the most potent class of drugs for the treatment of GERD.
Despite a high degree of efficacy, clinical failure in patients with GERD has been reported. In fact, the failure rate of PPIs has increased proportionally with the expansion of indications for their use. It is estimated that about 30% of GERD patients remain symptomatic when taking standard (once daily) dose PPIs. Of these patients, the majority will continue to experience GERD symptoms on even higher doses of PPIs.
PPI failure has become a very common occurrence in gastrointestinal (GI) practice and is increasingly seen at the primary care level. Furthermore, as more and more primary care providers feel comfortable prescribing PPIs as the first line of treatment for GERD, PPI failure will become even more common. in primary care practice. This is compounded by the increasing availability of PPIs as an over-the-counter (OTC) drug. Furthermore, the broader indications for PPIs and their frequent use by physicians for many upper gastrointestinal symptoms will inevitably lead to more treatment failures. Currently, PPI failure has become one of the major clinical challenges in GERD management that gastroenterologists must address in their practice almost daily.
1.1. Methods of Evaluation A review of the medical literature was performed to identify primary research and treatment centers aimed at evaluating the effects of PPIs in patients with GERD. Medline and PubMed searched for English-language articles published between 1985 and 2005. Terms used for online bibliographic searches included: PPI, GERD, esophagitis, Barrett's esophagus, esomeprazole , lansoprazole, omeprazole, pantoprazole and rabeprazole. Additional articles were identified through manual search and from other physicians and experts in the field.
1.2. Definition of PPI treatment failure Currently, the medical literature does not provide an accepted definition of PPI treatment failure. This is compounded by the common usage of the term “refractory GERD,” which is less specific but indicates a similar clinical situation. PPI studies typically lasted 8 weeks in erosive esophagitis and 4 weeks in non-erosive reflux disease (NERD) or symptomatic GERD. In the erosive esophagitis treatment trials, the primary clinical endpoint was symptom resolution and esophageal mucosal healing. In symptomatic NERD or GERD, symptom improvement is often the only clinical end point. Failure of PPIs in erosive esophagitis has been identified as a result of persistent esophagitis despite adequate PPI therapy. It was later recognized that healing of erosive esophagitis may not necessarily be indicative of complete resolution of GERD symptoms. In other words, patients may continue to have GERD symptoms even though the esophageal mucosa has completely healed (up to 15%). The percentage of patients who reported complete resolution of GERD symptoms despite persistence of esophageal erosions while taking PPIs is unknown. On the other hand, up to 50% of patients with symptomatic recurrent erosive esophagitis on once-daily PPI therapy had no evidence of concurrent recurrence of endoscopically manifest esophagitis.
In patients with NERD, traditional clinical endpoints such as complete resolution of GERD symptoms may not be achieved. A “miler” clinical end point was adopted in the NERD studies, allowing patients to experience some degree of symptoms. This can obviously vary from individual to individual, based on patient expectations from therapy, which can be influenced by gender, age, ethnic background, social status, education, nationality country of origin and other important demographic factors.
In a recent study of patients with untreated GERD, PPI failure was defined as patients who continued to report heartburn symptoms of any degree for at least 2 days/week for the past 30 days. In another study, treatment with a standard dose PPI was considered to have failed if the patient continued to experience heartburn more than once a week for the past 3 months.
For the purposes of this article, many authors propose the following definition of PPI failure: “Patients who are unable to fully heal their esophagus and/or respond to symptoms satisfactorily after a course of treatment. full standard dose PPI (once a day)”. This definition allows to include patients who find their remaining symptoms of PPI treatment to be bothersome, independent of frequency or severity.

1.3. Degree of Treatment Failure of PPIs While practice guidelines at US universities on GERD state that: "Medically difficult-to-treat GERD is rare", recent studies This has challenged this assertion. Inadomi et al evaluated 298 consecutive patients in a heartburn clinic and found that 42.3% needed more than a PPI once a day to control their symptoms. In a community-based clinical class I study of patients, Carlsson et al evaluated the efficacy of omeprazole 20 mg once daily in 225 patients with and without esophagitis. corrosion for a period of 4 weeks. After 4 weeks of treatment, 41% of patients reported complete symptom relief and 73% complete symptom relief. The study's authors suggested that 27% of all patients with GERD would continue once-daily PPI therapy after 4 weeks of treatment. A study of 11 064 patients with chronic heartburn showed that PPIs were the drug of choice in patients with GERD to prevent heartburn. However, only 58% of PPI recipients reported being completely satisfied with their anti-reflux treatment. The authors concluded that even with PPIs there is potential to improve treatment outcomes. In general, it is likely that PPI failure rates differ from those of NERD patients and those with erosive esophagitis. However, studies of different phenotypic manifestations of GERD suggest that the overall PPI failure rate is about 30%.
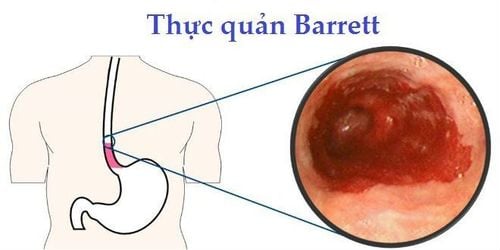
1.4. PPIs failure in different GERD groups To understand which patients are likely to fail PPI therapy, in this review we will separately evaluate three phenotypic manifestations of GERD: erosive esophagitis. (GERD), non-erosive esophagitis (NERD), and Barrett's esophagus (Figure 1). This is supported by natural studies, which demonstrate that most NERD patients (85–90%) do not progress overtime to develop erosive esophagitis or Barrett's esophagus and those with esophagitis Erosion is unlikely to progress overtime to Barrett's esophagus. It is essential to identify, from which, the phenotypic expression of GERD most patients with PPI failure. Identifying the primary source of this challenging patient population may help develop appropriate diagnostic techniques and better tailor therapy.
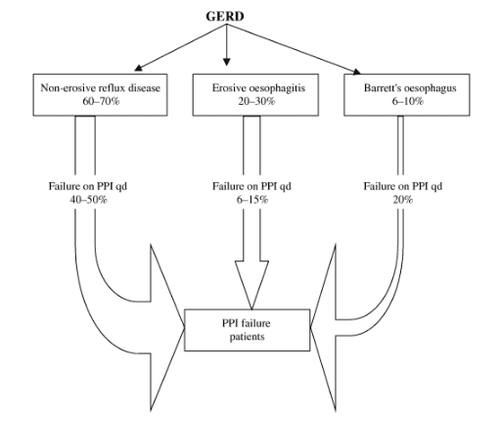
Proportion of patients who failed to take a once-daily proton pump inhibitor (PPI) in each gastroesophageal reflux disease (GERD) group. The non-erosive reflux disease (NERD) group, which accounts for most patients with GERD and has the lowest response rate to once-daily PPIs, is the major cause of PPI failure.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
F. Fass , M. Shapiro , Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease – where next? Alimentary Pharmacology and Theurapeutics, Volume22, Issue2, July 2005 Vaezi MF. ‘Refractory GERD’: acid, nonacid, or not GERD? Am J Gastroenterol 2004; 99: 989– 90. Richter JE, Bochenek W. Oral pantoprazole for erosive esophagitis: a placebo-controlled randomized clinical trial. Pantoprazole US GERD Study Group. Am J Gastroenterol 2000; 95: 3071– 80.