This is an automatically translated article.
Posted by Master, Specialist I Nguyen Thi Thanh Binh - Rehabilitation Doctor - General Surgery Department - Vinmec Danang International General Hospital1. Anatomy
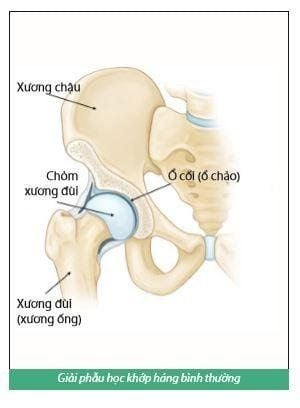
The hip joint is one of the largest joints in the body, consisting of the ball and socket. The socket is formed by the acetabulum, which is part of the large pelvis. The sphere is the femoral head, the upper end of the femur (tubal bone). The bony surfaces of the sphere and alveolus are covered with smooth articular cartilage that cushions the ends of the bones to allow them to move easily. Surrounding the hip joint is a thin layer of tissue called the synovial membrane. In a healthy hip, this membrane secretes a small amount of fluid that lubricates the cartilage and minimizes almost all friction during hip movement. Bands of tissue called ligaments (hip capsule) connect the ball to the socket and provide stability to the joint.
2. Common causes of hip damage
2.1 Osteoarthritis of the hip
Osteoarthritis is an age-related degenerative joint disease that causes wear and tear of cartilage in joints, often occurs in the elderly and is especially common in people with a family history of arthritis. The articular cartilage that cushions the bones in the hip is worn away, then the femoral head will rub against the acetabulum and break the cartilage, causing narrowing of the joint space, pain and leading to stiffness.2.2 Rheumatoid arthritis
This is an autoimmune disease in which the synovial membrane becomes inflamed and thickened. This chronic inflammation can damage joint cartilage and the bone under the cartilage, which in turn causes pain and stiffness.
2.3 Post-traumatic arthritis
This condition can occur after a fracture or severe injury to the hip joint. The femoral head breaks and the cartilage in the joint can be damaged, causing pain and stiffness over time.
2.4 Avascular tip necrosis
This is a condition where the femoral head is damaged due to a lack of blood supply to the femoral head. The lack of blood can cause the bone surface to sag, narrow the joint space and cause stiffness.
2.5 Abnormal structure of hip or lower extremities
Some infants and children have structural abnormalities in the hip or lower extremities. Although these problems can be successfully treated in childhood, joint damage can still occur later in life.
3. Indications for total hip replacement surgery
3.1. Pain
The most common reason for sick people to see a doctor is pain. Hip pain affects the quality of life of patients, most patients have pain when walking, gradually increasing pain even at rest and at night, when moving or standing for a long time. The most common site of pain is the front of the thigh, the inguinal fold, spreading to the lower front of the inner thigh, sometimes down to the knee joint, behind the buttocks or the femoral trochanter.
3.2. Limit movement
Decreased hip mobility gradually increases and affects daily activities such as difficulty in squatting, difficulty tying shoelaces, difficulty in going to the toilet, difficulty in dressing... Common hip flexion movements still good, while abduction, hip adduction and especially rotation are affected very early. Patients often have difficulty walking and limping because the hip joint bears the most body weight. However, the indication for total hip replacement is only given when the patient:
Constant hip pain, even at rest, day or night; Stiffness in the hip limits mobility. Other supportive treatments from anti-inflammatory drugs, physical therapy, or walking aids are still not enough to relieve pain. Patients with severe hip osteoarthritis stage IV Patients with late stage femoral head resorption (grades 3 and 4) Patients with femoral neck fractures or traumatic femoral head fractures. . . Had a hip replacement but had complications or didn't get the desired results MORE: Hip replacement - The optimal solution for people with severe femoral head loss
4. Rehabilitation program after total hip replacement surgery
Exercise as soon after surgery as possible to achieve joint range of motion and avoid complications from prolonged lying. That's why patients must start exercising as soon as they wake up in the recovery room. Early exercise also helps to increase circulation, reduce swelling of the operating feet, and avoid thromboembolic complications. To achieve the goal in exercise, it is necessary to understand, the patient's own efforts during the recovery period and the dedicated help of the physiotherapist technician. Physiotherapy technicians will come to the hospital bed to guide, usually 2 times a day, each session is about 30-45 minutes.
4.1. Goals to be achieved before discharge
Patients know to avoid bad postures that easily cause artificial hip dislocation Regain strength of the muscles around the hip and knee joints on the painful leg Prevent complications caused by lying in bed for a long time such as: embolism, pneumonia , skin ulcers, urinary tract infections, muscle atrophy, stiffness The knee joint is flexed and extended normally, avoiding the phenomenon of knee stiffness. The patient knows how to use crutches or a walker. Thus, the patient can walk in the room and go to the toilet by himself without fear of falling. The patient must know how to do the exercises independently so that when he is discharged from the hospital he can practice at home because the exercise program still lasts several months.
4.2 Points to note when doing physical therapy
Encourage the patient to practice active joint movement Exercise slowly, follow the breathing rhythm, ie breathe regularly and practice Must focus on muscle contraction exercises and must gradually increase active exercise If surgery to replace Cemented total hip joint: walking with crutches or a frame, the patient's leg can support the full load. The duration of crutches is 3 to 4 weeks. If total hip replacement surgery is not cemented: walking on crutches or on a frame, the painful leg may be able to support some of the body's weight. The duration of crutches is longer, usually 8 to 12 weeks. Use a pillow between your legs when resting or sleeping to avoid crossing your legs together. Knee immobilizer (Zimmer brace): may or may not be used, depending on whether the surgeon uses an anterior or posterior hip incision.
4.3 Preparation before surgery
Before surgery, each patient should fully prepare the following tools:
Walker: 01 or crutches 01 pair. Loafers or anti-slip socks: 01 pair. Pressure socks: 01 pair
4.4 Specific exercise program after surgery
1. Day One
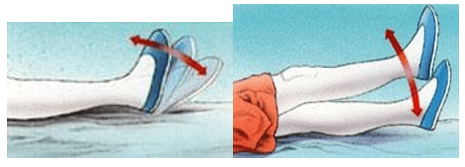
Exercise ankle movement, especially instep flexion: The patient lies on the bed, inhale deeply and flex the ankle, hold the flexed position for 5 seconds, then exhale and relax the ankle, rest. Rest for 5 seconds and then repeat the movement. Practice like this about 20 times. Straight leg lift: The patient lies on the bed, takes a deep breath and lifts the leg straight up about 40 cm from the bed. This movement helps strengthen muscles. Practice sitting up: The physiotherapist or family member helps lift the patient to sit up on the bed, or sit up and remove the legs from the bed. Sitting early helps the patient to be more comfortable and avoid complications of pneumonia and embolism. If the patient is elderly, on the first day, just practice sitting up in Fowler position (elevating the body at a 45-degree position relative to the bed). Patients practice deep breathing, lung capacity will increase. Exercise abdominal muscles: help patients urinate easily
2. Day 2
Continue to exercise ankle movement and straighten legs Practice leg extension: Lie on the bed, spread legs about 40 degrees with straight knees Practice knee extension and knee flexion without support: Patient sits up with legs out of wall bed for gentle knee flexion. Take a deep breath and raise your shins so that your knees are straight, hold that position for 5 seconds. Then exhale and release the knee joint to gently bend, rest for 5 seconds, then repeat about 20 times
3. The 3rd day to the end of the first week
Learn to walk with crutches or a support frame: By the third day, the patient begins to walk, usually with two crutches or a support frame. Older adults should use a walker because the frame has four legs, so they are less likely to slip and fall than with crutches. The surgical leg is allowed to bear the force while walking. The time to wear crutches depends on the type of joint used
4. The following weeks
The patient continues to do hip flexion and flexion exercises until the expected range of joint motion is knee extension, 90 degree hip flexion, and 40 degree hip flexion. At follow-up visits, the doctor will assess joint range of motion and will prescribe other movements to achieve maximum range of motion.5. From the fourth week
The patient begins to do exercises to strengthen muscles such as cycling in place. At first pedal with light tension then gradually increase depending on your condition

4.5 The movements should and should not be done in daily activities
Artificial hip replacement surgery helps relieve pain for the patient and improve the function of the hip that has been damaged before. So the artificial hip joint is never as perfect as the real human joint. Therefore, to protect the artificial joint well, the patient should pay attention to avoid some daily activities as follows:1.Do not bend your thighs into your stomach or bend your back too much, making the angle of your thighs and body less than 90 degrees
Do not sit on chairs without armrests, because this makes it difficult for the sick person to stand up No should stand up in this position (ie, stand up with legs in front) Before standing up, the patient must place the operating leg in front of the chair, the other foot under the chair, with both arms on the armrests of the chair. to get up.
When lying down, you should spread your legs, do not close the operating leg close to the middle axis of the body. Do not sit cross-legged When sleeping on your side, you should put a pillow between your legs, don't lie like this When going to the toilet: don't sit on a low toilet, you must sit on a high toilet Don't bend too low to pick up living items or wear socks Total hip replacement surgery for people with femoral head damage, aseptic head degeneration, or severe hip osteoarthritis has become common. . Thanks to this technique, many patients have restored hip function, can walk and live normally.
Currently, patients after performing hip replacement surgery can go to the Department of Rehabilitation - Vinmec International General Hospital for physical therapy and rehabilitation. The faculty has the strength of rehabilitation for patients after orthopedic trauma surgery, cardiac - thoracic surgery, stroke and pediatric respiratory rehabilitation.... In particular, Vinmec owns The team of doctors has specialized in Rehabilitation with many years of experience and dedication to patients. The subdivisions such as: medical examination area, physical therapy area, movement therapy area, ... are spaciously designed, equipped with many modern equipments, bringing a comfortable feeling for patients to collect. get the best treatment results. At the same time, the Department of Rehabilitation is also equipped with a system of therapeutic machinery from leading countries in technology such as the Netherlands, Japan, etc., which will bring satisfaction to customers to use. services of Vinmec.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.