This is an automatically translated article.
The article was written by Master, Specialist Doctor I Nguyen Thi Thanh Binh - Rehabilitation Doctor - Department of General Surgery - Vinmec Danang International General Hospital.Thoracic surgery rehabilitation is a very necessary treatment method with the aim of helping patients improve the functions that may be damaged during surgery such as the function of the respiratory system or the respiratory system. cyclic.
1. Outline
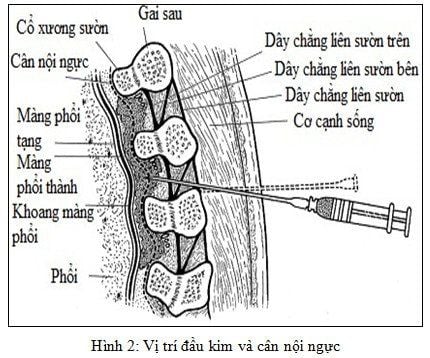
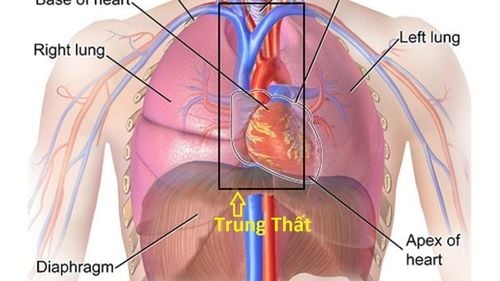
Thoracic surgery is usually indicated in the following cases:Malignancy : Primary bronchopulmonary cancer or metastasis from other places. Inflammation : Lung removal in the following cases: Pulmonary abscess, tuberculosis, bronchiectasis, aspergillosis, hydatid disease. Trauma: Stab wounds, gas wounds. Degenerative : Large lung bullae compresses normal lung tissue. Congenital: arteriovenous fistula, lobar emphysema. Types of thoracic surgery: Pneumonectomy: An entire lung is removed,. In the case of a radical pneumonectomy, the mediastinal lymph nodes and part of the thorax may also be removed. The empty space will be filled with a fluid rich in protein and fibrin. The size of the thoracic cavity is reduced due to lateral displacement of the trachea and heart, upward displacement of the diaphragm, and intercostal narrowing on the surgical side. Sometimes scoliosis develops later. Lobectomy: Any one of the five lobes can be removed; The right middle lobe and lower lobe lungs are often excised because of their common lymphatic drainage. If an upper lobe tumor invades the main bronchus, a segment of the main bronchus may be removed along with the lobe and the remaining lung and bronchus connected to the trachea. This surgery is called a sleeve lobectomy. Segmental resection: The lung segment is removed along with the segmental artery and bronchi. This surgery is often indicated for pulmonary tuberculosis but is rarely performed now. Wedge resection: This type of non-anatomical resection is used diagnostically in open lung biopsies and in the treatment of localized peripheral cancer in patients with reduced lung function. Most thoracic surgery is performed through the posterior-lateral incision. This line cuts the inferior fibers of the trapezius, dorsalis major, anterior dentate, and the internal and external intercostal muscles. The posterior extension also separates the great oblique muscle and the vertebral muscle group. Anterior-lateral thoracotomy is the basic modality of mitral valve enlargement and is used by some surgeons in pleurectomy.
Thoracic drainage: The purpose of drains in thoracic surgery is to remove fluid or air that may have accumulated inside. Drainage can be open or closed
Complications of lung surgery:
| Tại chỗ | Tổng quát | |
|
Sớm (0-2 tuần) |
Xuất huyết Xẹp phổi/ xẹp thuỳ phổi Nhiễm trùng vết thương Tràn khí do phẫu thuật Tràn dịch màng phổi Tích mủ màng phổi Dò phế quản-màng phổi Tổn thương dây thần kinh như dây thần kinh thanh quản quặt ngược, dây thần kinh hoành |
Thiểu năng hô hấp Rung tâm nhĩ Nhồi máu cơ tim Nghẽn mạch phổi/ huyết khối tĩnh mạch sâu Tai biến mạch máu não |
| Muộn |
Đau vết thương mở lồng ngực Tái phát ung thư Biến dạng thành lồng ngực Các cử động cánh tay bị hạn chế |
Ung thư di căn xa |
2. Physiotherapy/Rehabilitation (VLTL/PHCN)
2.1. Common problems after surgery The following problems may arise and need attention:Pain. Obstruction of the intercostal drain. Decreased intake of ventilation Congestion of secretions, phlegm Decreased range of motion, especially of shoulder on surgical side. Rib mobility is reduced. Bad posture. Reduced exercise tolerance It should be noted that the following treatment measures are generalizations only. Each patient must be evaluated individually for an appropriate plan. Treatment techniques and plans will vary depending on the patient's condition.
2.2. Thoracotomy The following plan is appropriate in cases of lobar resection, sleeve lobar resection and wedge resection, lobectomy, or simple thoracotomy (as in the case of a non-invasive tumor). resectable). Initially, the patient must be clearly explained to the patient about possible treatment options including incision, drainage, intravenous infusion, oxygen need and the importance of VLDL/rehabilitation.
2.2.1. Preoperative phase During the preoperative period, the physiotherapist may be involved in the general assessment of the patient's condition, particularly in the consideration of exercise tolerance.
Objectives:
The goals of preoperative physical therapy/rehabilitation include:
Maintain full range of motion and increase circulation by teaching active or active exercises with support for the arms, legs, and torso. me. Pay attention to exercise movement of the shoulder joint on the right side of the surgery because the open lung incision will cut the broad back muscle and full range of shoulder function may be lost. Active exercise guidance is needed that helps with shoulder lifting and arm flexion. Maintain correct posture by teaching patients to be aware of correct posture and sitting position. After thoracotomy, the patient tends to flex on the surgical side. That is lowering the shoulders and raising the pelvis because it is a less painful position
Maintain adequate ventilation by instructing breathing exercises to help the lung tissue maintain maximum expansion, and also to support breathing excrete sputum. Encourage general mobility by teaching the patient the best way to move around in bed. A bed tether is a useful aid Instruct patient on how to cough effectively with self-help as well as with the assistance of a therapist Teaches how to clear sputum with forceful breathing and coughing techniques . Program:
Instruction on flank breathing exercises (chest breathing). Diaphragmatic breathing (abdominal breathing) requires attention to the full range of diaphragm movement to prevent pleural adhesions. Effective cough exercises: to relieve pain, therapists can assist with manual manipulation. The thoracotomy can best be supported with the surgeon's hand pressing firmly on the thorax on the operating side in the sitting, lying, semi-reclining or side-lying position: Sitting on the front side is the most effective position for coughing, KTV should stand on the right side. The anterior and posterior sides of the thorax on the surgical side can be supported with hands, while the arms stabilize the entire ribcage and provide a “bear-hug” hold. - The patient must also understand how to stabilize the chest on their own during coughing by placing the hand of the healthy side around the ribs on the operating side as much as possible and applying strong pressure on the chest with the hand and forearm. The other hand aids the hug-support pattern by grasping the contralateral elbow to pull it firmly against the chest during coughing.

Ensure that the patient is given adequate pain medication. Make sure the drain is clear. Increase inspiratory ventilation with deep inspiratory exercises (costal and diaphragmatic breathing), asking the patient to inhale through the nose and hold air for a while in the supine position and lie on the right side (surgery side facing up). ). Also practice breathing in the same way in the prone position on the side of 450 and lying on the back on the side of 450. Reduce the stagnation of secretions by: (a) Vibrating the side of the chest below the incision.
(b) Elevate the foot of the bed to help drain waste and pleural fluid and air as needed.
(c) Breathe hard and cough with good support in a sitting position on your front side or on the edge of the bed.
Maintain joint range of motion and muscle strength of the arm and shoulder on the surgical side by doing a full range of active hand-assisted exercises. Prevent residual immobility syndrome with active leg, ankle and foot exercises, and early mobilization as soon as the drains stop aspirating. Patients should be encouraged to walk around carrying their own drainage vessel in their carry-on bag.
Prevent bad posture by: body training, shoulder belt and correct posture correction. Program :
Day of surgery:
Patients usually give oxygen for the first few hours after the patient is transferred to the room. Although the patient remains sedated, active shoulder support exercises should be performed to the fullest extent. Because the incision that cuts the back muscle is wide, these exercises must be performed immediately to prevent shortening and scarring of the muscle.
Patient performs breathing and coughing exercises with help. KTV firmly but gently supports the surgical side, taking care not to press directly on the incision and drain. Remind patients that exercises should be continued each time they wake up from sedation.
The first day after surgery:
The treatment program should be followed, first ensuring the patient is placed in a comfortable position when lying on the side.
To achieve this position, the patient should sit on the front side and the clinician standing on the surgical side and rearrange the cushions. The patient rotates to a supine position toward the healthy side; The patient's weight must be supported at the shoulders as they lower the body to the elbow and then lower to the side.
Place cleats for maximum comfort and support for the drain. If the patient is tilted posteriorly against the pillow (supine, 450-degree side), the anterior chest wall is free and facilitates bilateral rib movement while maintaining clear drainage of the operative lateral lung. If the patient is leaning forward on the pillow (pronation, 450 side), unimpeded posterior chest wall movement
The following three day treatments are necessary provided the patient is given medication to reduce full pain:
In the morning the patient should get out of bed as long as possible. Encourage the patient to perform breathing, coughing, arm, leg, and shoulder girdle exercises. Maintain correct posture throughout the day. Day 2 after surgery:
Thoracic treatment should be performed two or three times depending on the chest radiograph and auscultation.
When the patient is able to sit in a chair, perform core exercises. As soon as the drain is stopped, have the patient practice mobility and immediately add to the program of climbing and descending stairs if possible.
From day 3 until discharge:
Patients need to be assessed daily throughout the week. Enhance the program with posture exercises and general activities. Patients can be discharged 8-10 days after surgery; VLTL follow-up is not necessary except for specific shoulder problems.
2.3 Lung resection 2.3.1. Preoperative period: The patient was discussed about surgery and it was suggested not to lie on the healthy side for about 10 days after surgery. This will prevent fluid in the thoracotomy space from coating the bronchial stump, thereby reducing the risk of suture rupture that can lead to a bronchopleural fistula. Moreover, if the patient lies on the side of the healthy lung, their respiratory pattern will be disturbed. Since coughing creates a posterior pressure and can damage the bronchial stump, it is advisable to teach the patient how to breathe heavily and encourage them to do so to gradually expel the secretions before coughing lightly to clear it up. airway.

Ensure that the patient is adequately analgesia. Ensure good ventilation on the right side by: deep inhalation exercises (breathing on the right side and diaphragmatic breathing) through the nose and holding the breath in a sitting or semi-reclining position. Relieve stagnation of secretions by: (a) Vibrating one side of the healthy side during exhalation.
(b) Breathe vigorously with good protection of the incision.
Maintain range of motion and muscle strength of the shoulder joint on the surgical side by doing full range of active/active shoulder support exercises. Prevent rest-associated immobility with active leg, foot, and ankle exercises. Prevent poor posture by: (a) Bilateral diaphragmatic and flank breathing exercises.
(b) Body, shoulder and posture exercises.
Improve motor endurance by moving early with the diaphragmatic breathing pattern while walking (breathing exercise
4). Program :
When the patient comes back from the operating room, they will be given oxygen for the first few hours and given fluids.
Depending on the surgeon, they may have the drain clamped, and will almost certainly be removed every hour for a short period of time. The patient should not cough when the drain clamp is removed because a lot of fluid will be expelled and this can cause mediastinal displacement with consequent cardiac arrhythmias.
The treatment program starts from the day of surgery. In addition to general monitoring, the radiologist/VLTL must also check for a deficiency between apical and radial pulses because these patients may have atrial fibrillation due to excessive mediastinal displacement.
It is only necessary to place the patient in the supine position if the remaining lung requires drainage. Since drainage must be on the incision site, great care must be taken in positioning as described previously.
In general, these patients are discharged about 10 days after surgery but they may need extra help at home. Family members should be well informed about these patients so that they can prepare appropriately before the patient is discharged.
2.4. Pleurectomy and pleurectomy (decortication). Starting immediately after surgery should be given adequate analgesia to support rehabilitation treatment. The intercostal tube should never be clamped because the stagnation of air and fluid in the chest will prevent the lungs from sticking to the thoracic wall.
Postoperative program as described in thoracotomy and started on the day of surgery.
Take care of the drains with flank and diaphragmatic breathing exercises, and cough is deployed in the supine position with the surgical lung on top, the foot of the bed elevated.
The patient needs to work very hard to regain maximum function of the diaphragm and ribs. There can be a great deal of limitation of thoracic activity prior to pleural dissection due to empyema, so increased postoperative thoracic activity is required.
Encourage the patient to get out of bed on the first day and suggest walking immediately if possible.
Perform all progressive exercises and continue postural drainage until the drainage tube is removed.
Walking, stair climbing and general exercises should continue until discharge, when all movement is unrestricted and an upright position is achieved.
If the patient is young and has undergone pleurectomy due to pneumothorax, thoracic performance, lung function, and exercise tolerance are not desirable, they should be an outpatient of the rehabilitation department. .
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.