This is an automatically translated article.
The article is professionally consulted by Master, Doctor Phan Ngoc Toan - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital.1. Definition
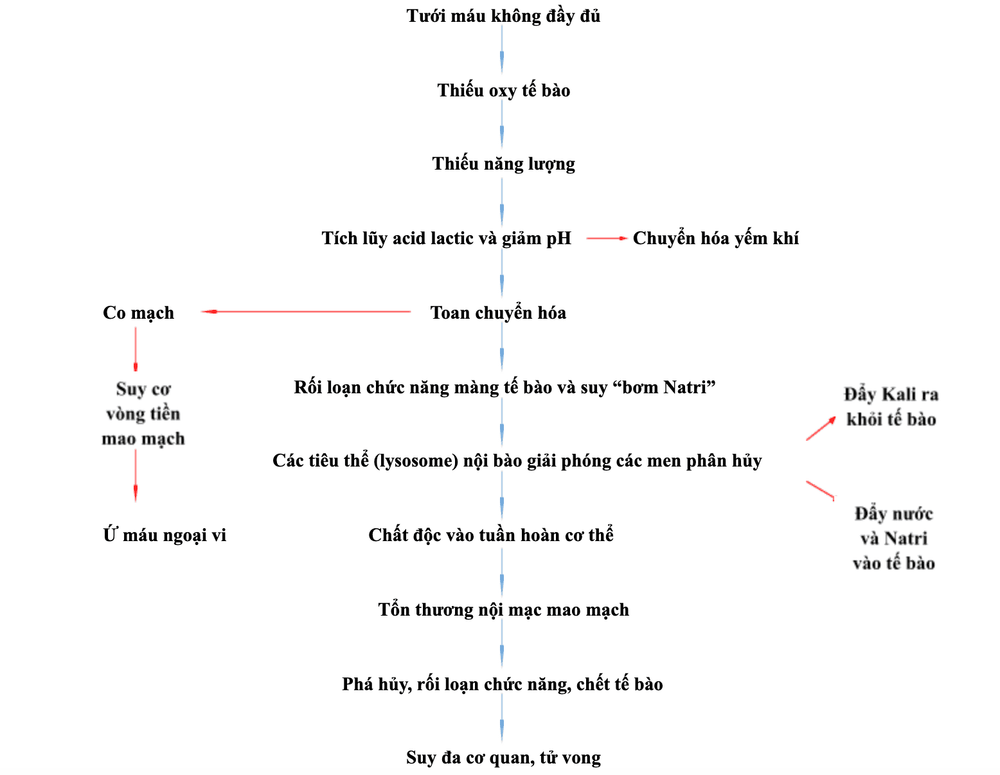
Acute circulatory failure (ACF) is defined in a number of ways, based on biochemical indices, hemodynamic indices, target organ dysfunction, or a combination of these findings.Circulatory failure can be defined as a life-threatening, generalized acute failure due to tissue hypoperfusion, resulting in cellular dysfunction due to hypoxia (anaerobic metabolic activity), loss of Physiological independence of oxygen supply and consumption, which is associated with increased lactate concentrations.
2. Pathophysiology
3. Cause
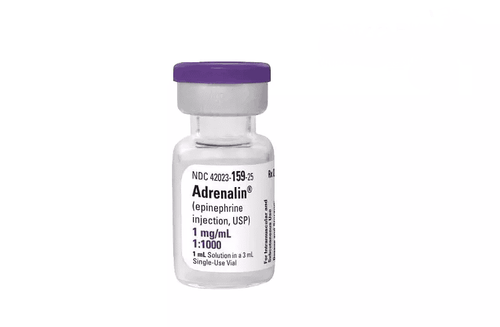
There are usually 3 main causes:The heart does not pump enough blood or is not strong enough (heart failure): Heart attacks and heart valve problems are common causes Blood vessels can dilate too much and blood is pumped up. redistributed from the heart to the rest of the body (known as distributive shock). Allergic reactions, serious infections, and shock that sometimes follow a spinal cord injury can all lead to circulatory failure. Not enough blood to pump around the body: Severe blood loss and prolonged vomiting or diarrhea can reduce blood volume to the point where blood pressure cannot be maintained. Inflammation after a severe burn injury can also cause blood volume to drop drastically.
4. Clinical manifestations
Acute circulatory failure progresses in stages and changes depending on medical interventions, which can basically be summarized as followsEarly stage:
Also known as compensated phase, the body has compensatory mechanisms with decreased organ tissue perfusion🡪 release of catecholamines, increased activity of the renin-angiotensin system, sympathetic nervous system activation causing selective vasoconstriction, blood shunts to the heart and brain Increases myocardial contractility to raise blood pressure. Due to insufficient oxygen source, the body will switch to anaerobic metabolism, increasing the production of lactic acid 🡪 Rapid detection through a portable blood gas analyzer Due to a compensatory mechanism, in the early stages of shock, patients may not show obvious symptoms, blood pressure has not decreased. However, tachycardia, mild changes in arterial blood pressure, or mild to moderate elevation of blood lactate are early manifestations of ACF Stage of Shock:
This condition occurs when the body's compensatory mechanisms are disrupted. overload and begin to show signs of dysfunction. Manifestations at this stage include symptoms such as tachycardia, small, difficult to catch, shortness of breath, irritability, sweating, acidosis due to increased lactic acid, low blood pressure, little urination, cold and moist skin.

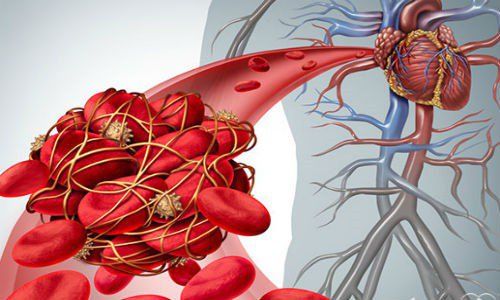
This is the final stage of shock, also known as Multiorgan Dysfunction Syndrome (MODS or Multiorgan Failure Syndrome MOFS) Manifesting progressive dysfunction of at least 2 organs, followed by It is life threatening for the patient. When this happens, it can affect and lead to many signs on organs such as: Lungs: Increased membrane permeability leads to effusion in the alveoli, severe can be resistant to O2 therapy. respiratory failure; Kidney: Decreased blood flow to the kidney leads to acute tubular necrosis, acute renal failure causes anuria and increased blood creatinine levels; Heart: Reduced blood flow to the coronary arteries, decreased myocardial contractility, decreased cardiac output, and decreased blood pressure can cause arrhythmias. Formation of a pathological spiral; The condition manifests in the organs and is accompanied by severe hyperlactatemia, which is resistant to therapeutic measures leading to coma. Death often occurs during this stage of shock.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.