This is an automatically translated article.
Article by Master, Doctor Mai Vien Phuong - Gastrointestinal endoscopist - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.
Gastrointestinal diseases are common after renal transplantation and can present with a variety of clinical and histological features. The diagnosis of post-renal inflammatory bowel disease is challenging because there are no definite histological criteria.
1. Overview
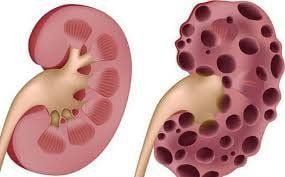
Kidney transplantation is considered the gold standard treatment for people with end-stage kidney disease, which significantly improves the patient's quality of life and survival time.
Gastrointestinal diseases are common after renal transplantation and may present with a variety of clinical and histological features. The diagnosis of post-renal inflammatory bowel disease is challenging because there are no definite histological criteria.
At the same time, the management of post-transplant inflammatory bowel disease can also be difficult due to the current use of immunosuppressive therapy, which may increase the risk of infectious complications. Furthermore, the clinical course of post-transplant inflammatory bowel disease may be more severe than that of general inflammatory bowel disease.
2. Prognosis of kidney transplant in patients with inflammatory bowel disease
Clinical course of inflammatory bowel disease presenting with flares and remissions. Intestinal and extra-gastrointestinal manifestations may include:
Renal failure Amyloidosis AA IgA nephropathy. These complications can even lead to kidney failure requiring a kidney transplant, although kidney failure is a rare complication, particularly in patients with Crohn's disease. Age and duration of inflammatory bowel disease are not risk factors for developing kidney failure. There is an association between oxalate nephropathy and inflammatory bowel disease because the prevalence of calcium oxalate urolithiasis in Crohn's patients is 5 times higher than in the general population. Furthermore, Crohn's disease appears to be a predisposing factor for hemolytic-uremic syndrome because of recurrent gastrointestinal infections. Few studies have reported the outcome of kidney transplantation in IBD patients who develop end-stage renal disease. In one study, a total of 21 patients with inflammatory bowel disease (12 patients with Crohn's disease and 6 patients with UC as well as 3 patients with other unspecified disease) received kidney transplantation. An additional 28 cases were reported in a French multicenter study.
3. What do the studies say?
Schnitzler et al. reported that 6 patients with inflammatory bowel disease (5 patients with Crohn's disease and 1 patient with UC) received kidney transplantation. The female/male ratio was 5/1 and the mean age was 54.1 years. Three patients were treated for inflammatory bowel disease prior to transplantation (primarily 5-ASA and steroids) and underwent ileostomy and fistula resection. At the time of kidney transplantation, all patients were in clinical remission. 3 patients required treatment for inflammatory bowel disease after transplantation (2 patients with Crohn's disease were treated with steroids and 6-MP and one patient with UC was treated with 5-ASA plus steroids). Interestingly, of the three patients who required post-transplant treatment, 2 received pre-transplant therapy. 1 patient had post-transplant lymphoproliferative disorder and one patient had kidney transplant cancer. At median follow-up was 112.5 months.4. Increased risk of re-hospitalization and death in kidney transplant patients with inflammatory bowel disease
In the series by Grupper et al., 12 patients with inflammatory bowel disease (7 patients with Crohn's disease and 5 patients with UC) received kidney transplantation. Men were more likely to receive kidney transplants than women, and the mean age was 48.4 years. IgA nephropathy and autosomal dominant polycystic kidney disease are the most common causes of end-stage renal disease. When compared with this rate in the matched control group, the rate of late re-hospitalization was significantly higher in the inflammatory bowel disease group. Furthermore, patient survival was significantly lower in patients with inflammatory bowel disease, with an estimated 5-year survival rate for patients of 80.8% compared with 96.8% for patients with inflammatory bowel disease. and no inflammatory bowel disease, corresponding to a risk-to-death ratio with the active graft of 1.41.
An increased risk of re-hospitalization and mortality associated with increased rates of infection, possibly due to poorer nutritional status in patients with IBD compared with patients without inflammatory bowel disease, has been demonstrated. by lower BMI and hemoglobin levels or as a consequence of higher levels of chronic immunosuppression because of treatments associated with inflammatory bowel disease. Interestingly, most patients remained in clinical remission or did not experience impaired response after transplantation, possibly as a consequence of more severe immunosuppression in the kidney transplant group compared with the liver transplant group. , in which the recurrence rate is higher. However, in patients whose inflammatory bowel disease recurred after transplantation, the median time to exacerbation after transplantation was 17 months, and CMV infection increased the risk of recurrence.
5. Conclusion
Gastrointestinal complications are common after kidney transplantation and they have a broad clinical spectrum, ranging from diarrhea to post-transplant inflammatory bowel disease. Chronic immunosuppressive drugs may increase the risk of post-transplant infection, drug-related injury, and may also be a cause of inflammatory bowel disease in immunosuppressed renal transplant recipients. Distinguishing the different forms of post-transplant colitis is challenging, as most have similar clinical and histological features.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: Gioco R, Corona D, Ekser B, Puzzo L, Inserra G, Pinto F, Schipa C, Privitera F, Veroux P, Veroux M. Gastrointestinal complications after kidney transplantation. World J Gastroenterol 2020; 26(38): 5797-5811 [PMID: 33132635 DOI: 10.3748/wjg.v26.i38.5797 ]