This is an automatically translated article.
The article is professionally consulted by Master, Doctor Le Xuan Thiep - Radiologist - Department of Diagnostic Imaging - Vinmec Ha Long International Hospital. The doctor has extensive experience in the field of diagnostic imaging.Acute limb ischemia is a sudden decrease in limb perfusion, with onset usually within 2 weeks, and has an impact on limb preservation. Currently, angiography and treatment of acute thrombus removal of the extremities digitized extremity is the most commonly used form to treat this pathology.
1. Symptoms of arterial occlusive disease caused by acute thrombosis of the limb arteries
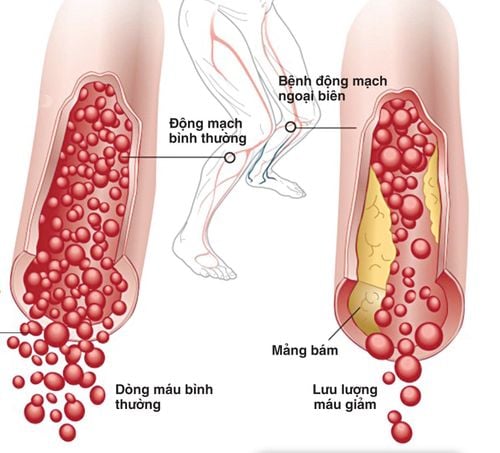
The first symptom of acute arterial thrombosis of the limb is a change in skin color in the extremities. A blocked limb artery will cause the skin in the ischemic limb to turn pale and have purple spots appear scattered.Next, the patient may develop sudden and severe pain in the occluded extremities; Feeling numb like ants crawling, gradually the patient will lose the feeling of depth in these extremities. The patient's extremities are also colder than the non-occlusive side because the thrombus cannot circulate in the artery.
In addition, the patient may also experience loss of pulse below the blocked artery or muscle paralysis when the artery is blocked for a long time.
Động mạch chi bị tắc sẽ làm cho vùng da ở chi bị thiếu máu tái nhợt đi và có đốm tím xuất hiện rải rác
2. In which cases is the acute extremity artery thrombectomy and treatment indicated?
The process of angiography and treatment of acute thrombus removal of the extremity digitized extremity is often used to determine the status of thrombosis to provide appropriate treatment. Specifically, this method is indicated for acute arteriovenous thrombosis of the extremities (< 3 weeks) or the thrombus length is not more than 3cm.3. When is contraindication to imaging and treatment of acute arterial thrombosis of the extremities?
The angiography and treatment of acute thrombectomy with digitalization of the background are necessary to determine the patient's condition. However, there are some special cases where this method cannot be used, the doctor will appoint the patient to use the more suitable method. The cases are:Patient has chronic arterial-venous thrombosis of the extremities (> 3 weeks). The clot is more than 3cm long. The patient is allergic to iodinated contrast agents. Patients with severe renal failure (grade IV). Severe and uncontrolled coagulopathy. Pregnant.

Chống chỉ định chụp và điều trị đối với bệnh nhân suy thận nặng
4. What should the patient prepare before the procedure?
The patient will be thoroughly explained by the doctor or nurse about the procedure for the best understanding and coordination.Before performing the imaging and treatment of acute arterial thrombosis of the extremities, the patient should fast for 6 hours and only drink less than 50ml of water.
When brought into the intervention room, the patient will be placed on his back, fitted with a monitor to monitor breathing, pulse, blood pressure, electrocardiogram, SpO2. The nurse will disinfect the procedure area and then cover it with a sterile cloth with holes.
5. Procedure for imaging and treatment of acute arterial thrombosis with digital erasure
Step 1: Anesthesia methodThe patient is placed supine on the scanning table and the first intravenous line is placed. Usually, the doctor will use 0.9% isotonic saline to place the line. The patient will be given local anesthesia, but in some cases, general anesthesia will be required such as young children who are not conscious of work or patients who are too excited or scared.
Step 2: Insert the tube into the vein
After the patient is anesthetized, the tube will be placed into the vein. The location or direction of the vascular opening depends on the location of the patient's thrombus and the purpose of the physician's intervention.
Usually, the doctor will use a 21G micro-needle set to poke the vessel through ultrasound guidance, then place the tube into the vessel.
Step 3: Angiography to assess the damage
Step 3 is the step to take and evaluate the damage, the process of angiography of the limb system will be done through the catheter. The doctor will use the obtained images to evaluate the entire vascular system above and below the thrombus.
Step 4: Treatment intervention
After assessing the extent of damage, the doctor begins the treatment intervention by inserting a specialized catheter into the clot and conducting aspiration of the thrombus under negative pressure by hand or by machine. These manipulations will be repeated until the clot is completely aspirated.
Step 5: Monitor while aspirating the thrombus
The patient will be taken to the ward for monitoring after the procedure to remove the thrombus. During this time, medical staff need to adjust the infusion rate for the patient based on the results of the coagulation test or as directed by the interventional doctor.
Step 6: Recanalization after thrombus aspiration
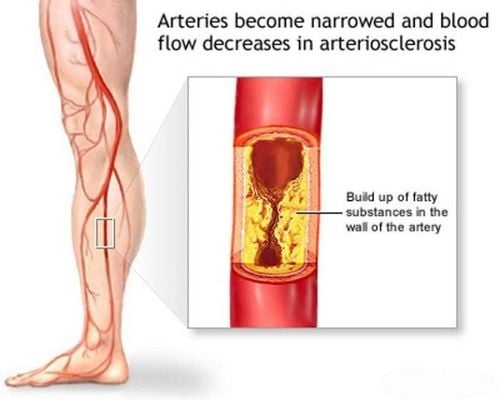
If the thrombus site is still narrow or atherosclerotic plaque causes narrowing of the vessel lumen, the patient will be assigned angioplasty or stenting. Doctors can also use both methods at the same time if necessary.
Step 7: Evaluation after intervention
Finally, the patient will have an angiogram to evaluate the circulation after completing the manipulations. The doctor will close the access to the vessel and end the procedure.
Acute limb ischemia is one of the most serious clinical conditions for peripheral vessels. This condition can directly affect the ability to preserve limbs and the morbidity and mortality of patients. Therefore, the patient needs to be taken and treated for acute thrombus removal of the extremities in a timely manner.
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. examination and treatment at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORELower extremity atherosclerosis: Signs and treatment Lower extremity artery disease: How is it treated? Beware of lower extremity peripheral artery occlusion