This is an automatically translated article.
Patients infected with Covid-19 may experience mild to severe health problems called post-Covid-19 complications. Myocarditis is one of them. The World Health Organization (WHO) has issued warnings about this dangerous disease. Early diagnosis as well as timely and proper treatment can limit the negative effects of post-Covid-19 myocarditis on patients' health.
1. What is myocarditis?
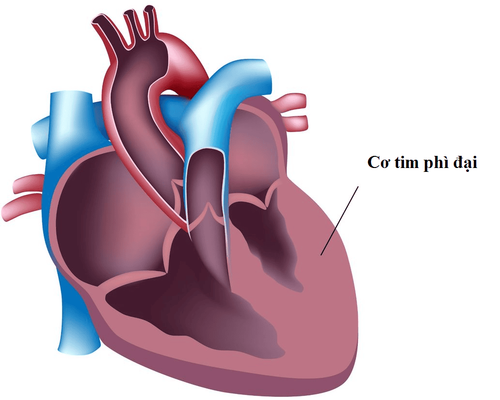
Myocarditis is a cardiovascular disease characterized by necrotizing inflammation of cardiac muscle cells. If left untreated, it can lead to permanent damage to the heart muscle leading to dangerous cardiovascular complications. The heart muscle can be directly damaged by pathogens such as viruses, bacteria or fungi...2. Post-Covid-19 myocarditis
2.1. Risk factors Acute respiratory syndrome SARS-CoV-2 (Covid -19) was originally considered a respiratory disease, but it is now recognized as a complex multisystem disease. Patients with COVID-19 myocarditis have the same risk factors as those with severe COVID-19.
Serious complications and death in COVID-19 patients are related to old age and comorbidities, including diabetes, cardiovascular disease, and respiratory disease. About 50% of patients with severe COVID-19 have at least one of these risk factors. Similarly, 58% of patients with myocarditis due to COVID-19 had at least one of the comorbidities such as hypertension, diabetes, obesity, and asthma or COPD.
2.2. Epidemiology Prior to COVID-19, the incidence of myocarditis was between 1 and 10 cases per 100,000 persons per year. The highest proportion of patients is in men aged 18 to 30 years. Interestingly, most cases of myocarditis in the highest risk group were in healthy and active people.
According to the US Centers for Disease Control and Prevention, the risk of developing myocarditis after contracting COVID-19 is much higher, with 146 cases per 100,000 people. The risk is higher for men, older adults 50 years of age or older, or children younger than 16 years old
2.3. Pathogenesis The SARS-CoV-2 virus, after entering the body mainly through the respiratory tract, will be introduced into the blood through gas exchange in the lungs, then the virus will find its way to the heart and myocardium. Here, the SARS-CoV-2 virus binds to the cell membrane protein angiotensin converting enzyme 2 (ACE2) that regulates the receptor that ultimately leads to apoptosis, the release of viral and cardiac antigens. These antigens, when immobilized to antigen-presenting cells (APCs), lead to the release of interleukins (IL1, IL6, IL12, TNF alpha), which, when presented to CD4 + T helper cells, are CD8 + T cells and B cells. These substances, when released in excess, cause a phenomenon called a Cytokine storm, which activates a strong inflammatory process in the heart muscle to destroy antigens (SARS-CoV-2 virus). ) and lead to destruction of cardiac muscle cells.
3. Diagnosis of post-Covid-19 myocarditis
3.1. Clinical Symptoms Common clinical manifestations of COVID-19 infection are fever, cough, dyspnea, and fatigue. The World Health Organization has identified fever and cough as prominent features of COVID-19. Fever, shortness of breath, and chest pain are typical manifestations of myocarditis that tend to overlap with symptoms of COVID-19, thus making diagnosis difficult. In addition, in myocarditis can manifest through the following clinical symptoms:
Arrhythmia, fast or slow heart rate. Auscultation: Blurry heart sound in T1 or both T1, T2. Apical systolic murmur, galloping sound. Symptoms of heart failure appear in patients with severe myocarditis. 3.2. Subclinical Electrocardiogram Sinus bradycardia or sinus tachycardia. Cardiac arrhythmias: Atrioventricular block, extrasystoles, atrial fibrillation... ST segment elevation or depression, low amplitude QRS complex, flattened T wave. Blood tests A blood count indicates inflammation. Biochemical tests such as: Cardiac enzymes, NT-Pro BNP, CRP, Ferritin, D-dimer ... Echocardiography Cardiac dysfunction. Ejection fraction decreased. Ventricular hypertrophy, the chambers of the heart can dilate, is a functional regurgitation of the heart valve. Mechanical regurgitation of heart valves. Blood clot images. Pericardial effusion. Computed tomography CT-scan, magnetic resonance imaging (MRI), straight chest X-ray: Enlarged heart shadow. Pulmonary venous congestion. Pericardial effusion, pleural effusion. Cardiac biopsy or histopathology: The most common findings are multifocal or diffuse lymphocytic infiltration in the myocardium and endothelium with edema and myocardial necrosis. Other findings included a positive anti-SARS COV nucleocapsid protein antibody, myocardial hypertrophy, multiple ischemic sites, and thrombosis with left atrial and left pulmonary artery thrombosis in one patient.
4. Treatment of post-Covid-19 myocarditis
4.1. Medical treatment Corticosteroids: Immunosuppressive drugs, used to treat myocarditis caused by the SAR-CoV-2 virus. Medicines to treat heart failure caused by myocarditis: Using beta-blockers, diuretics, ACE inhibitors, angiotensin II receptor blockers (ARBs)... Can help lower blood pressure, reduce fluid body and reduce pressure on the heart. Antiarrhythmic drugs: Help control the heart rate and reduce the risk of blood clots that are common in atrial fibrillation. Specific treatment: Specific drugs to treat Covid-19 have been researched and developed, but the effectiveness of these drugs has not been confirmed yet. Therefore, patients need to consult their doctor before deciding to use. 4.2. Surgical treatment Cases of severe post-Covid-19 myocarditis that do not respond to medical treatment, or have progressed to dangerous complications, may be indicated for surgical treatment including surgical treatments, including: :
Ventricular assist device (VAD): This device supports pumping blood from the ventricles of the heart to organs in the body, indicated for cases of myocarditis with severe heart failure complications. Ventricular support is used while waiting for other treatments such as a heart transplant. Aortic balloon counterpulsation: Helps increase blood flow and relieve pressure on the heart. Exchange of oxygen across the extracorporeal membrane with an ECMO machine: The ECMO machine works like a human lung but outside the body. ECMO is often indicated for patients with severe heart failure awaiting a new heart transplant. Heart transplant: Heart transplantation is considered a last resort for patients with very severe myocarditis, severe heart failure, almost total damage to the myocardium, and unresponsive to all of the above treatments. .
5. Backup
Prevent myocarditis by:
Avoid close contact with someone who has the flu or other respiratory illness until the patient has recovered. Patients who develop symptoms of Covid-19 infection should try to avoid contact with others. Regular and proper hand washing is one of the best ways to prevent Covid-19. Vaccination: Vaccination is recommended against COVID-19, other myocarditis-causing agents such as influenza and rubella . However, there are now reports of a small number of cases of myocarditis following vaccination with the COVID-19 vaccine. Therefore, it is necessary to consult with your doctor before deciding to receive any vaccine. Covid-19 is a dangerous and complicated disease that can lead to dangerous complications, including myocarditis. The prevention of Covid-19, early diagnosis and proper treatment of post-Covid-19 injectable myositis can contribute to limiting dangerous complications as well as reducing the mortality rate for patients.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.