This is an automatically translated article.
The article was professionally consulted by Specialist Doctor II Pham Thi Tuyet Mai - Obstetrician and Gynecologist - Department of Obstetrics and Gynecology, Vinmec Hai Phong International General HospitalNearly 50% of women over 40 years old have urinary incontinence, 40% of women over 50 years old have prolapsed pelvic organs. Pelvic organ prolapse is not life-threatening but greatly affects a woman's daily life, causing women to lose confidence and comfort.
1. What are pelvic floor problems?
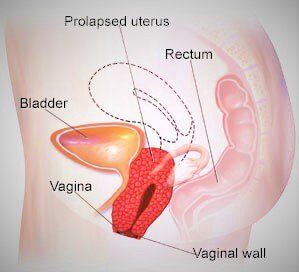
Pelvic organs include vagina, uterus and cervix, urethra, bladder, rectum and small intestine. These organs are supported by the muscles and ligaments of the pelvic floor.
The role of the pelvic floor is to keep these organs in place, not to fall down when doing heavy work, running and jumping. The pelvic floor also plays the role of opening and closing the openings of the urinary tract, vagina and anus, helping to control bowel movements and urination at will, sexual activity, and making the birth process easier. These three systems work in harmony with each other, each giving way to the other under the active control of people.
Aging with age, time can cause the function of muscles and ligaments to weaken, slip out of their original position and lead to phenomena such as uterine prolapse, bladder prolapse or rectal prolapse. ; More severe may be stretched, torn, affecting the function of the pelvic floor. Possible health problems in the pelvic floor are related to weak pelvic floor muscles, pelvic organ prolapse. This condition will get worse over time and can cause dangerous complications if not treated promptly.
2. Common symptoms of pelvic floor diseases
Many women don't notice or experience specific symptoms because they don't see any difficulty with pelvic organ prolapse. And most women see this change from mild to severe. Specifically, clinical symptoms may be encountered as follows:
Lower urinary tract: Urinary incontinence, increased frequency of urination, weak or prolonged urine flow, hesitancy, feeling of incomplete voiding, need must act to bring the internal organs back into the vagina to be able to urinate or defecate. Pelvic organ prolapse : Feeling of vaginal bulge, feeling of pressure and heaviness in the pelvic floor and vagina, seeing or palpating a vaginal or pelvic floor bulge; Using tampons also becomes difficult. Sexual disorders : painful sex, shallow, deep, hindered, decreased sensual desire, wide vagina. Anorectal disorders: Urinary incontinence, or urgency, urinary urgency, urinary urgency, defecation, feeling of incomplete defecation, constipation, decreased rectal sensation, appearance of substance Mucus discharge from the rectum, rectal bleeding. Pain in the urinary tract and pelvic organs : Pain in the bladder, urethra; pain in the vulva, vagina, perineum; pelvic pain (may be cyclical), groin pain; lower back pain; Tension or pain in the lower abdomen or around the pelvis.
3. What causes women to have pelvic floor problems?
Most of the causes of pelvic floor prolapse are due to childbirth. Most women who give birth vaginally are more likely to have pelvic floor health problems than those who have a caesarean section.
When you enter the time of delivery, the muscles that support the pelvic organs are stretched to the limit, leading to these muscles quickly weakening. Another cause of pelvic organ prolapse is the drop in estrogen hormone levels before and after menopause. This makes the body deficient in the amount of collagen needed to support the pelvic connective tissue.
Some other causes of pelvic floor damage:
People who have undergone pelvic surgery. Women enter menopause in old age: lack of estrogen causes muscle fibers to atrophy, stiffen and lose elasticity. Aging of pelvic muscles and ligaments. Women participating in physical activities. Factors that increase abdominal pressure: people who are overweight or obese, people who are often constipated or have a chronic cough, people who often wear a bra. Abnormal pelvic floor structure, the parts move under the influence of contraction force. Nerve conduction abnormalities. Obstetric trauma: straining at birth when the cervix is not fully dilated, perineal tear is not fully restored... Genetic factors.
4. Classification of pelvic floor prolapse problems
Pelvic floor visceral prolapse has many different forms such as:
Uterine prolapse: The uterine part has the phenomenon of prolapse into the vaginal area, causing the vagina to be compressed. Vaginal prolapse: The top area of the vagina is prolapsed. This condition is common in women who have had a hysterectomy. Rectal prolapse - when the rectum pushes out of the vagina. Bladder prolapse: The bladder area drops deep into the vaginal area due to the weakening of the pelvic floor muscles, which can't hold in their normal position. Prolapse of the urethra: When the urethra protrudes into the vagina. Often, prolapse of the bladder will occur concurrently with this phenomenon. Small bowel prolapse: A bulge appears in the back wall of the vagina, that is, the small intestine is pushed into the back wall of the vagina. This phenomenon often occurs concurrently with vaginal prolapse.
5. Diagnosis and treatment of pelvic floor prolapse problems
Examination and diagnosis of pelvic floor prolapse Patients should see a doctor if you have difficulty urinating, vaginal bleeding, or any of the above symptoms. The location and medical condition can be different in many people. Always discuss with your doctor to determine the best method of diagnosis, treatment and management for you.
The doctor will do a physical and pelvic exam including a vaginal and rectal exam to diagnose disease or perform blood and urine tests if needed. The doctor may ask the patient to stretch or perform a strong cough to check the bladder elasticity, urine leakage, urine to be expelled completely. bladder or not. In addition, your doctor will also order you to perform an ultrasound and an X-ray of the urethra and bladder when urinating (VCUG) for a more accurate diagnosis.
Treatment of pelvic organ prolapse It is necessary to avoid straining when defecating, avoid lifting heavy objects, avoid coughing a lot and avoid being constipated. Eating foods rich in fiber can help treat constipation. Practice Kegel exercises to improve the condition. If Kegel exercises don't work, you need physical therapy. For postmenopausal women, hormone replacement therapy can be used to help tone muscles. If the above methods still do not work, surgery or the use of supportive devices will be performed to treat pelvic floor organ prolapse.
6. Risk of pelvic floor disease

Anyone can get this disease. However, rectal prolapse mostly occurs in women. You can limit your chances of getting the disease by minimizing your risk factors. Please consult your doctor for more information.
Factors that can increase your risk include:
Being overweight or obese; Frequent lifting of heavy objects; Persistent cough; Straining to defecate (due to constipation); Cancer. Just because you don't have risk factors doesn't mean you can't get the disease. The above signs are for reference only. You should consult a specialist for more details.
7. Methods to reduce symptoms of pelvic floor disease without surgery
Obstetrics - During pregnancy: Avoid weight gain, constipation, avoid squatting, proper toilet posture.- During childbirth: Listen to the doctor's instructions on lying position, how to push, in case you really need to use forceps, you can have a cesarean section to avoid pelvic floor diseases.
- Postpartum period: Apply cold, avoid edema, infection, breastfeed to stimulate uterine contraction, do pelvic floor exercises, eat enough green vegetables and fruits to avoid constipation.
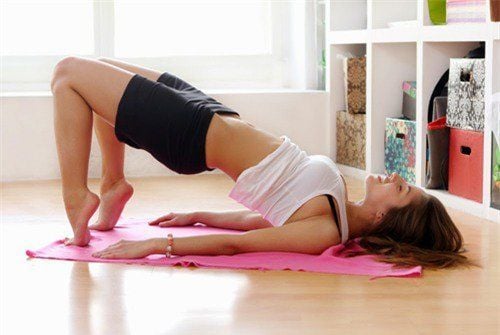
Exercises to do Abdominal breathing, pelvic floor exercises, cross-abdominal exercises, transverse and straight abdominal exercises, kegels, knack.
Kegel exercises - Helps to squeeze the urinary cessation organ, helps muscles and ligaments around the vagina, urethra, or rectum to be flexible, improves urinary incontinence. You should do it at least 3 times a day.
- Practice in all positions and at your leisure, as soon as you remember
- Practice contractions and holdings: Perform a gradual contraction to the maximum and hold for 3-10 seconds, rest for 4 seconds, continue to repeat keeping the interval 5 times until the muscle is tired and can't continue to contract. Rest for 2 minutes, switch to quick contractions.
- Fast muscle contraction, maximum strength and immediately relax: Each contraction is fast for at least 10 beats or until the muscle is tired and can't continue to contract.
Lifestyle changes - When experiencing urinary incontinence: should limit drinking water, drink only enough, limit caffeinated beverages because caffeine is a diuretic.
-When having intestinal problems: Should add fiber, limit the problem of constipation and unwanted contractions in defecation. Besides, you can visit your doctor to use more laxatives and stool softeners.
Exercise for the bladder You can eat and drink according to the specified time frames so that urination also takes place at the specified times. This testifies to the urinary incontinence being overcome.
Slimming Losing weight or losing fat will help your overall health become more comfortable, reducing the risk of pelvic organ prolapse.
Vaginal cap Cap or pessary. These are very special instruments, they are inserted deep into the vagina to support the support of all pelvic organs.

8. Treatment of common pelvic floor problems after childbirth
8.1. Medical treatment Indications: The cases of organ prolapse grade 1-2 have no complications and have not affected personal life.
Treatment: - Change appropriate living habits.
- Supplementing with topical estrogen such as vaginal tablets or topical creams...
- Physical therapy to restore pelvic floor
- Lifting of the bladder, uterus, and rectum into the vagina and conditioning urinary incontinence treatment.
8.2. Surgical treatment Indications: - Pelvic floor organ prolapse from grade 2, with symptoms or complications, affecting quality of life.
- Treatment with vaginal cap for 3-6 months failed.
- The patient requires surgery.
Treatment: - Restore the structure and physiological function of the prolapsed organ in the pelvic floor.
- Indications for hysterectomy when there is pathology of the uterus and cervix.
Aging causes pelvic floor muscles to weaken and pelvic organ prolapse occurs. This condition is common in women who have given birth vaginally, so to avoid it happening to you, you can do simple methods to help prolong the elasticity of the pelvic floor muscles.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.