This is an automatically translated article.
Posted by Doctor Tran Truong Giang - Intensive Care Unit - Vinmec Times City International Hospital
Pericardial effusion has many causes, depending on the extent we have different interventions and different attitudes. In particular, with acute pericardial effusions is an emergency that requires immediate drainage of pericardial fluid to release because there is a risk of immediate death. Pericardial drainage is an emergency procedure that requires fast, decisiveness and high accuracy. Because the procedure itself can cause fatal complications.
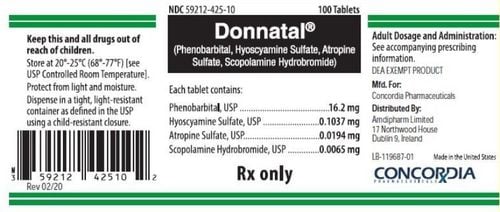
1. What is pericardial drainage?
Pericardial puncture is the insertion of a needle into the pericardial cavity and through that needle a catheter (catheter) to aspirate or drain fluid in order to reduce the pressure in the pericardial cavity rapidly with Acute compression or delayed drainage with chronic pericardial effusion, or for the purpose of determining the cause of effusion pericarditis by fluid color as well as hematological, biochemical, and bacteriological tests of the pericardium outside the heart.

Chọc dò lấy mẫu bệnh phẩm để xét nghiệm dịch màng ngoài tim
2. Indication for drainage of pericardial fluid
The doctor will appoint pericardial drainage in the following cases:
Acute tamponade due to pericardial effusion: An urgent indication, absolutely, without delay, immediately. Pericardial effusion in patients with cancer therapy. Pericarditis with fluid, without clinical symptoms of tamponade, to determine the cause
3. Procedure for drainage of pericardial fluid in resuscitation
Step 1: Preparation:Patient: It is necessary to be explained to see the need to conduct the procedure of puncture and drainage, the patient needs to calm down to cooperate. The patient's family needs to be fully explained about the benefits of the procedure, the risks, events and complications that may occur during the procedure and need to sign a consent to perform the procedure on the patient. sick. Means - tools: Sterile instruments: Put in a sterile tray covered with sterile towels, 1 probe needle: 5-8cm long, 2mm in diameter, 1 syringe 5ml and needle for anesthesia, 1 syringe 20ml or 50ml, 1 towel with holes and 2 towel clips, 1 pericardial catheter with lock. Use drainage in case of a lot of fluid, 1 Kocher forceps, 1 cup and tubercle swabs, 1 central venous catheter placed by Seldinger technique, several square gauze pads, 2 pairs of gloves. If you keep gloves in a bag, keep them separate. Clean tools and medicines (Vials of iodine alcohol 1%, alcohol 70o, anesthetic: Novocain, Xylocaine 1-2%, atropine: 2 ampoules; Seduxen 10 mg 1 tube, adhesive tape, bandage scissors, holder for 3 test tubes with labeled (including 1 sterile tube), clearly stating name, age, department, room, test sheet, medical record, sphygmomanometer, stethoscope, stopwatch...). Other equipment... Medical staff: Procedure crew includes at least 1 doctor and 2 nurses

Chuẩn bị phương tiện và dụng cụ trước phẫu thuật
Step 2: Technical procedure
The patient is in the lying position with the head elevated, breathing oxygen and continuously monitoring the parameters: Heart rate, electrocardiogram, blood pressure, breathing rate, arterial blood oxygen saturation on monitoring . Ensure SaO2>90% when performing the procedure Insert a peripheral venous line with a sufficiently large diameter of the needle (the catheter) and firmness. If an echocardiogram is available, a bedside echocardiogram should be performed immediately prior to the procedure to re-evaluate the extent of the pericardial effusion and re-determine the puncture site and the direction of the needle. needle depth to be safe and effective for the patient. If the patient does not have much difficulty breathing, IM injection of 5 - 10 mg of Morphine and subcutaneous injection of 2 ampoules of Atropin 0.25 mg to prevent vagal reactions during the procedure. After that, disinfect the puncture site on the patient's chest, spread a sterile dressing, the doctor washes his hands, puts on a sterile shirt and gloves, and begins the procedure. Anesthetize the needle puncture site with Xylocaine from shallow to deep in layers: skin, subcutaneous and muscle. There are 2 commonly used puncture sites in clinical practice: Marfan line and Dieulafoy line.
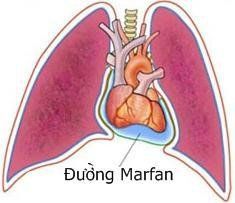
Đường chọc dò Marfan
The puncture point is 3-4 cm from the sternum, about 1 cm to the left of the sternum. First, use a fine needle to probe the actual depth into the patient's pericardial cavity. Point the needle up and back, the needle is tilted about 20-300 compared to the skin surface, while walking, the doctor gently sucks the syringe and brings the needle to the middle of the left collarbone. The needle will touch the pericardial cavity 2-5 cm deep. Determine the direction and depth of the probe needle. Use a needle to place a central venous catheter in the direction of the newly withdrawn probe needle for the purpose of inserting the catheter into the pericardial cavity to aspirate and drain fluid. Simultaneously insert the needle and aspirate as before with the probe needle. Close to the specified depth, the physician needs to quickly observe the patient and electrocardiogram. If the fluid cannot be aspirated, gently push the needle a little deeper, pushing and aspirating the syringe at the same time. If the patient cooperates well, the patient can now be told to hold his or her breath for a few seconds before inserting the needle into the pericardial cavity at the pre-explored depth.

Đưa kim chọc dò vào khoang màng ngoài tim
When the fluid is easily aspirated into the syringe, the physician fixes the iron needle and gently pushes the plastic sheath into the needle. When the plastic tube is 2-3 mm deep, the doctor will pull out the iron needle and continue to push the plastic needle-coated tube deep into the pericardial cavity. When the iron needle has been completely removed from the outside, the doctor inserts the catheter into the lumen of the plastic tube and inserts it about 15cm deep into the pericardial cavity. After checking, draining fluid easily through the catheter, then remove the above plastic tube from the patient's chest and fix the catheter to drain the pericardial fluid. Connect the catheter to an infusion line and insert the infusion line into an isotonic infusion bottle after the fluid has been drained to form a closed, sterile drainage system. Adjust the above-mentioned infusion line lock so that the pericardial fluid does not outflow excessively and rapidly to avoid hemodynamic disturbances. Increase infusion rate when pericardial fluid has drained above 200 ml and signs of tamponade are clinically relieved to avoid cardiac emptying due to inadequate return to the heart during diastole.

Luồn catheter dẫn lưu dịch màng ngoài tim
4. Possible Complications
Sympathetic shock: When the needle passes through the pericardium, suddenly the patient's blood pressure drops, pale skin, slow heart rate. Immediately think of sympathomimetic shock, raise the patient's leg to make it easier for blood to return to the heart, and inject 2 ampoules of Atropin 0.25 mg under the skin. If the heart rate is still less than 50 beats/min and the blood pressure is still low, an intravenous infusion of adrenaline with the dose to increase blood pressure is indicated and a booster injection of Atropin with the above dose is indicated. Need to differentiate with right ventricular needle puncture when pericardial fluid is blood, especially when probe is lemon yellow, but when puncture with catheter needle, it is blood, especially when the blood clots in the syringe. must have poked the right ventricle. When unsure, an echocardiogram should be performed immediately. Right ventricular puncture: A potentially serious event with perforation of the ventricular wall, requiring prompt and precise management. Sudden electrocardiographic changes, blood infiltrating and coagulating in the syringe, and rapid and rapid hemodynamic changes are signs of right heart chamber puncture. Bedside echocardiography with contrast technology allows for a better understanding of this condition (contrast is not present in the pericardial cavity, but may instead be present in the right heart chamber). It is necessary to shock the patient, transfuse blood and macromolecule fluids, and contact surgery if the clinical condition, hemodynamic status does not improve but worsens. Right coronary puncture: Bright red blood and clots in syringe. Usually the amount of blood drawn into the syringe is not much, then the needle occlusion can no longer be withdrawn and does not cause serious hemodynamic disturbances. Need to withdraw the probe and start again after re-evaluating the patient's general condition. Cardiac Arrhythmia: Usually causes supraventricular arrhythmias such as paroxysmal supraventricular tachycardia, extra-atrial fibrillation. These arrhythmias usually pass quickly if the pericardial fluid is drained and the patient has less dyspnea.

Chọc vào động mạch vành phải có thể gây rối loạn nhịp tim
Infection : Rarely infection at the pericardial puncture site. Severe infections are often pulmonary in origin (accompanied by pulmonary abscesses causing leakage into the pericardial cavity). Pneumothorax: rare. The patient feels sudden chest pain, decreased alveolar murmurs, and drum beats are signs to think of pneumothorax, especially when the entrance is at the special locations mentioned above. If the condition allows, it is still advisable to continue to carry out the procedure of pericardial drainage, then take a straight chest X-ray to decide on the management attitude: aspiration and pneumothorax if indicated.
5. Taking care of the sick
Clinical: Pulse, blood pressure, respiratory rate, arterial oxygen saturation, central venous pressure, urine every 30 minutes / 1 time in the first 2 hours after puncture, 3 hours / 1 time in 24 hours next. Subclinical: Electrocardiogram, echocardiogram Change tampons where drainage is placed daily Health counseling and education before and after the technique To protect cardiovascular health in general and detect early signs of heart attack and stroke, customers can sign up for Cardiovascular Screening Package - Basic Cardiovascular Examination of Vinmec International General Hospital. The examination package helps to detect cardiovascular problems at the earliest through tests and modern imaging methods. The package is for all ages, genders and is especially essential for people with risk factors for cardiovascular disease.
Customers can directly go to Vinmec Health system nationwide to visit or contact the hotline here for support.
MORE
The dangers of pericardial effusion Diagnosing pericardial effusion Decoding common chest pain