This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Le Duc Hoang - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International General Hospital.Emergency pericardiocentesis indicated in case of acute chest compression due to pericardial effusion; pericarditis with effusion, to determine the cause and contraindications for pericardiocentesis when the pericardial effusion is small.
1. What is pericardiocentesis?
Pericardial aspiration is a procedure in which a needle is inserted into the pericardial cavity to drain the fluid out of the patient's body. This method is used when the patient has pericardial effusion and is considered a cardiovascular emergency. The phenomenon of pericardial effusion is a phenomenon of increased secretion of the pericardium, when the secretion is much, it will cause pressure on the heart due to the pericardial fluid covering the outside. The heart fails to expand during diastole, resulting in a decrease in cardiac output.Causes of pericardial effusion are:
Pericardial effusion due to cancer Pericardial effusion due to trauma, after heart surgery Heart perforation, heart rupture Complications of coronary intervention, caused by Heparin Causes other such as pericardial tuberculosis, pericarditis Pericardial effusion after myocardial infarction Due to pathology: Systemic disease, hypothyroidism, systemic edema
Chọc dò màng ngoài tim do tràn dịch màng tim
1.1 Pericardial effusion in the absence of cardiac compression
Usually no clinical symptoms, but sometimes patients present with negative pain heaving, heavy chest pressure. Small amounts of pericardial effusion are often difficult to detect on physical examination. Massive pericardial effusion may show faint heart sounds, Edward's sign, and pulmonary rales secondary to compression. On the electrocardiogram, there will be diffuse low voltage signs. Alternating electrical signs are common in cases of pericardial effusion. Echocardiography can most clearly diagnose and monitor pericardial effusion. 1.2 Pericardial effusion when there are signs of cardiac compression
The patient feels restless, anxious or agitated, lethargic, and may faint; Decrease in urine volume, shortness of breath, feeling of chest compression; Collapse, anorexia and emaciation in cases of chronic pericardial effusion. Increased central venous pressure, tachypnea, tachycardia, pericardial rub, faint heart sound. Symptoms similar to right heart failure: Hepatomegaly, jugular venous distension, possibly associated pleural effusion. Blood pressure measurement showed a drop in blood pressure and the inversion sign was defined as a drop in blood pressure of less than 10 mmHg when the patient took a deep breath. Echocardiography reveals fluid in the pericardial cavity (indicated by echocardiographic gaps). Left ventricular hypertrophy.
2. Indications and contraindications for pericardial puncture in the emergency
Indications for emergency pericardiocentesis when:Acute tamponade due to pericardial effusion: Is an indication for emergency pericardiocentesis. Pericarditis with fluid, to determine the cause: Indications can be considered, delayed to monitor and consider more carefully before proceeding. Contraindications for pericardiocentesis in the emergency:
Small degree pericardial effusion
3. Pericardial puncture procedure

Thực hiện chọc dò màng ngoài tim
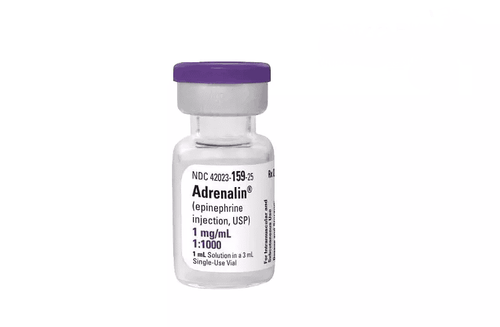
Step 2: Prepare clean tools and medicine including: 2 pairs of sterile gloves and 1% iodine alcohol, alcohol 70; anesthetic; atropine: 2 ampoules; Seduxen 10 mg 1 ampoule; adhesive tape, do not cut the tape; rack for 3 test tubes with labels, 1 of which is sterile, clearly stating full name, age, department, and room; test sheets, medical records; monitor electrocardiogram, blood pressure, breathing rate, SpO2; first aid equipment; Echocardiogram machine and some other necessary tools
Step 3: Put the patient in a supine position, breathe oxygen, monitor SpO2 and ECG and place an intravenous line.
Step 4: Bedside echocardiography immediately before the procedure to re-evaluate the extent of the pericardial effusion and re-determine the site of the puncture.
Step 5: Place a peripheral intravenous line. Use 9% sodium chloride solution to keep the catheter unclogged. In case the patient does not have much shortness of breath, Seduxen is injected intramuscularly and Atropin is administered subcutaneously to prevent vagal reactions during the procedure.
Step 6: Carry out extensive disinfection of the puncture site on the patient's chest, put on a sterile dressing, the doctor washes his hands, wears a sterile shirt and gloves. Then anesthetize the needle puncture site with Xylocaine from shallow to deep layer by layer: skin, subcutaneous and muscle.
Step 7: Punch and drain the pericardium with a Marfan puncture. The puncture point is 1-3 cm from the sternum, first probe with a fine needle. Point the needle up and back, the needle is tilted about 20-30 degrees compared to the skin surface, while walking, the doctor gently sucks the syringe and brings the needle to the left shoulder. When the needle touches the pericardial cavity after 2-5 cm deep, the doctor inserts the needle into the pericardial cavity, and at the same time aspirates the fluid.
Step 8: When the fluid is easily aspirated into the syringe, the doctor fixed the iron needle and gently pushed the plastic tube that covered the needle deep into the pericardial cavity. From this point on, the technique is similar to that of a central venous catheter. After withdrawing the iron needle completely, the doctor inserts the catheter into the plastic tube and inserts it deep into the pericardial cavity. After checking, withdrawing fluid easily through the catheter, remove the plastic tube from the patient's chest and fix the catheter to drain the pericardial fluid.
Step 9: Connect the catheter to an infusion line and an infusion bottle to form a closed, sterile drainage system. Adjust the above-mentioned infusion buckle so that the pericardial fluid does not outflow too much and rapidly to avoid hemodynamic disturbances.
Master - Doctor Cao Thanh Tam has many years of experience in diagnosing and treating cardiovascular diseases; Performing transthoracic echocardiography in the field of internal medicine and interventional Cardiology; Perform other non-invasive functional investigations in the diagnosis and treatment of cardiovascular diseases. Currently working as a cardiologist at Vinmec Central Park International General Hospital since November 2015.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE
SEE MORE
Dangers of effusion pericardial effusion Diagnosing pericardial effusion Decoding common chest pain