This is an automatically translated article.
The article was professionally consulted with Master, Doctor Le Phuc Lien - Urologist - Department of General Surgery - Vinmec Central Park International General Hospital.Penile removal without lymphadenectomy is the most common treatment for penile cancer that is detected at an early stage.
1. Penile cancer overview
Penile cancer is cancer that occurs on the penis in men. Cancer arises from the nonkeratinizing squamous epithelium of the foreskin and glans mucosa. This is a common disease in men over 40 years old, accounting for 6-8% of all cancers.Cancer of the penis has the following manifestations:
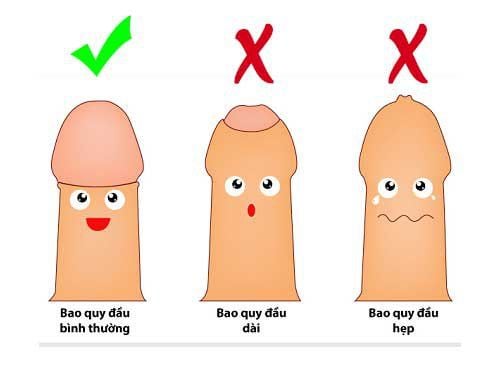
Tumor appears on the surface of the glans, the inner surface of the foreskin or the groove of the foreskin; Warts bleed easily when cleaning, having intercourse; Tumor spreads gradually around, ulcers; In case of narrowing of the foreskin, malignant tumor is hidden, difficult to detect. In the early stages, the tumor is small, with symptoms of itching at the tip of the penis, prolonged foul discharge, pain when urinating, touching, intercourse, ... The cause of penile cancer is mainly due to the narrowing of the foreskin. head, the penis is not cleaned properly, leading to the formation of genital warts, prolonged inflammation and easy development of malignant tumors. In addition, people with genital diseases such as penile inflammation, have benign tumors in the penis or have sexually transmitted diseases such as genital warts, ... also have a high risk of cancer. penis.
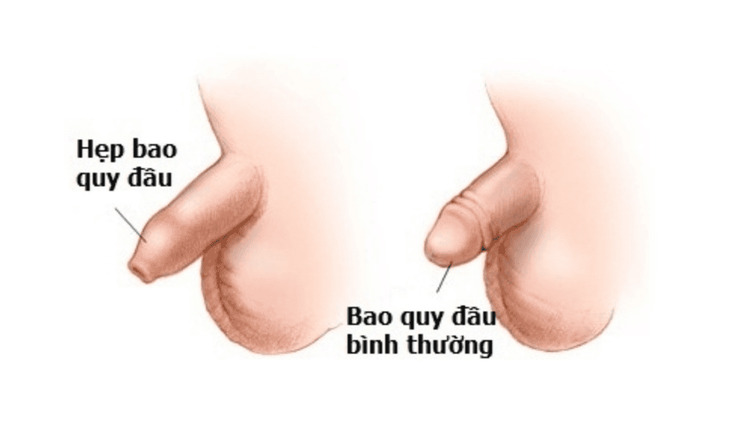
Hẹp bao quy đầu là nguyên nhân hàng đầu gây ung thư dương vật
2. Learn about the method of penis removal without lymph node dissection
Penileectomy without lymphadenectomy is also known as partial penileectomy without lymphadenectomy. This method is often used in the treatment of penile cancer in men detected at an early stage.2.1 Indications/Contraindications Indications
Penile cancer at stage T1a (tumor invading the submucosa but not lymphatic vessels, not low differentiated), no bilateral inguinal lymph nodes palpable; Penile cancer at stage T1b (tumor with invasion of submucosa and lymphatic vessels, low differentiated), bilateral inguinal lymph nodes are not palpable; Penile cancer stage T2 (tumor invading cavernous or spongy), bilateral inguinal lymph nodes are not palpable: should be considered. Contraindications
Penile cancer at stage T3 (tumor invading the urethra) or higher; Patients with bilateral inguinal and femoral lymph nodes should consider indications; Patients with contraindications to surgery in general: Liver failure, progressive severe renal failure, blood clotting disorders,... 2.2 Performing surgery Preparation
Performer: Surgical team (specialist, 2 surgical assistants) and anesthesiologists (anaesthesiologists, anesthesiologists, equipment staff, support staff); Patients: Need to ensure records (basic tests, electrocardiogram, chest X-ray, urinary tract ultrasound, inguinal and pelvic lymph node system ultrasound, biopsy confirmed penile cancer); be clearly explained about the purpose, procedure and risk of complications of surgery; improve physical and psychological condition; stable treatment of medical diseases (diabetes, high blood pressure); fasting, enema, cleaning the surgical area; can use prophylactic antibiotics before surgery if indicated; Means: Surgical kits, specialized sutures, urinary catheters, urine bags; Estimated time: 45 - 75 minutes. Perform
Patient position: Supine; Doctors and support staff in the right positions; Endotracheal or spinal anesthesia; Assess tumor location and tumor invasion; Make an incision around the circumference of the penis; urethral dissection , threading the wire marking the urethra to determine the part of the urethra to be cut; dissect 2 cavernous objects to the position to be cut; remove cancerous lesions of the penis with cavernous bodies, spongy objects, and urethra to the end of the entire lesion, ensuring that the healthy part remains; Stitching to stop bleeding 2 cave objects; bring the urethra out and fix it to the skin of the penis; close the skin of the penis; Insert a urinary catheter and bandage the incision.

Cắt dương vật không vét hạch phải được thực hiện theo đúng quy trình
Monitor the patient's overall condition and bleeding status; Antibiotic treatment, reduce inflammation, relieve pain; Monitor hematoma and urethral bleeding within the first 72 hours; Urinary catheters can be removed 7-10 days after surgery. Management of complications
Bleeding after surgery: In case of heavy bleeding, the incision needs to be reopened to check and stitch to stop the bleeding; Edema of the skin of the penis body: Treat by making incision to drain the compression fluid; Urethral stricture : Can reopen the urethra to the skin or perform bladder drainage ; Urethral fistula: A rare complication. However, if the patient has a lot of urethral fistula, causing fluid accumulation and perineal infection, it is necessary to re-operate to manage the lesion. When being assigned to perform penileectomy without lymphadenectomy, patients need to strictly follow the doctor's instructions to ensure the best treatment effect and minimize the risk of unwanted complications.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Recommended video:Free surgery for children with genital defects at Vinmec