This is an automatically translated article.
The article was written by MSc Vu Duy Dung - Doctor of Neurology, Department of General Internal Medicine - Vinmec Times City International Hospital.A primary writing tremor is a specific movement tremor that occurs mainly or only during writing and not at all or infrequently in other movements or movements involving the hands.
1. Run writes primitive
This definition of primary tremor excludes patients with dystonic postures accompanied by hand tremors during writing (i.e. dystonic tremor).The disease can be sporadic or autosomal dominant. Primary tremor has a frequency similar to that of essential tremor (ie, 4 Hz to 8 Hz), and it is reduced with ethanol administration in 30% to 50% of patients.
The underlying mechanism of primary write run is unknown; It is disputed whether it represents a variant of essential tremor or a variant of focal dystonia, and there are families with all three of these conditions.
Treatment of primary tremor includes propranolol, primidone, and anticholinergics (trihexyphenidyl 2 mg/day to 10 mg/day) as well as the use of orthopedic and writing devices. Intramuscular botulinum toxin has also shown some benefit, as has localized surgery in a limited number of patients. Eventually, some patients switch to writing with the other hand.
2. Run standing position
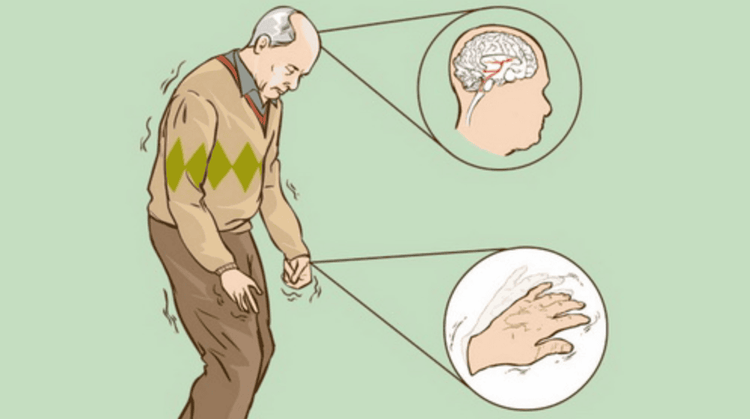
This is a rare syndrome characterized by unsteady standing and high-frequency tremors in the legs. Onset is typically in the 6th decade of life.Although most cases are sporadic, rare familial cases have also been reported. Patients are more likely to experience unsteadiness while standing than tremors. Because of these symptoms, patients often avoid situations where they have to stand (eg, standing in line).
Indeed, they will eventually sit down or walk away after a short time (seconds to minutes), depending on the severity of the illness. As the disease progresses, tremors may begin to invade the standing phase during walking. On examination, the patient may see or feel a slight and rapid tremor (14 Hz to 16 Hz) in the calves. Because of its high frequency and small amplitude, orthostatic tremor can be difficult to appreciate with the naked eye.
In some cases, tremors can be heard when a stethoscope is placed on the trembling calf, the sound is like a helicopter in the distance. EMG shows 14 Hz to 16 Hz copper tremor in the leg muscles (especially in the calves). A slower tremor of greater amplitude may also overlap this tremor peak, which may represent a secondary harmonic of the high-frequency tremor, and this may be more disabling for the patient than the rapid tremor. Many cases are in the context of the comorbidity of Parkinson's disease.
Treatment of orthostatic tremor is challenging. Many drugs have been used and are often less effective. The most commonly used drugs are clonazepam (0.5 mg/day to 4 mg/day), gabapentin (300 mg/day to 1800 mg/day), and carbidopa/levodopa (25 mg/100 mg/day to 250 mg/day). 1000 mg a day). Many other drugs have also been tried, including propranolol, primidone, phenytoin, carbamazepine, ethosuximide, baclofen, and acetazolamide, although because of their rarity no large clinical trials have been performed. DBS surgery may also be beneficial for some patients.
3. Cerebellar tremor
The term classic cerebellar tremor is used to describe tremors that may occur in patients with cerebellar ataxia and other classic disorders of cerebellar origin.Today, cerebellar tremor has become a separate type of tremor equivalent to involuntary tremor. This is a type of tremor that occurs with movement toward the target (eg, the finger-nose-finger test) and worsens as the target is approached.
However, cerebellar tremors (ie, tremors of cerebellar origin) do not always present separately as involuntary tremors. Indeed, the clinical phenomenological origin of cerebellar tremor is heterogeneous, and it extends beyond voluntary tremor to include postural, kinesthetic, resting tremor, and orthostatic tremor. This heterogeneity is consistent with the early work of Holmes, who described many types of tremor in addition to voluntary tremor in cerebellar lesions.
On examination, patients with classic cerebellar tremor often have other cerebellar signs, including glancing abnormalities, dysarthria or broken speech, gait ataxia, and hypotonia. When these patients are examined, it is important, although often difficult, to filter out tremors (i.e. rhythmic and pulsating movements) from symptoms of efficiency and timing of movement. (meaning confusion); Both occur during the finger-nose-finger maneuver, but the former usually improves with DBS surgery, whereas the latter may worsen.
Many drugs have been used to treat cerebellar tremor, although their effectiveness is limited. The most effective treatment for severe cerebellar tremor is hippocampal DBS surgery, as discussed above.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles source reference:
Louis ED. Tremor. Continuum (Minneap Minn) 2019;25(4, Movement Disorders): 959–975.














