This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital
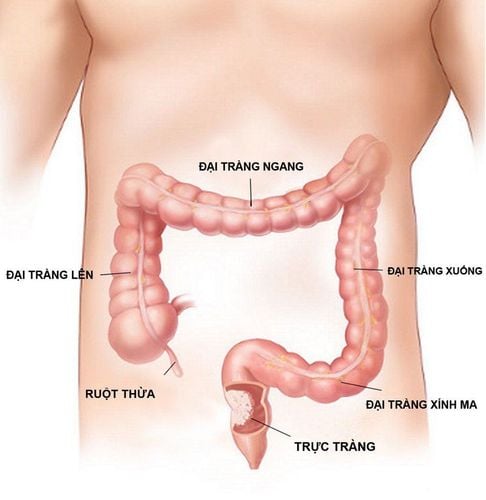
Hemorrhagic ulcerative colitis (CRC) is a chronic inflammatory bowel disease affecting the colon with an unclear pathogenesis. Research on this pathology has mainly developed in the last 100 years, however, in the literature, the record of a pathology characterized by diarrhea and having similar properties to CAP has been described since long.
In the consensus of the Crohn's and Colitis Organization (ECCO) in 2017, it was agreed to define this as a chronic inflammatory disease causing persistent inflammation of the colonic mucosa with histopathological characteristic of granulomatous lesions. The disease affects the rectum and colon to varying degrees with each progression and remission.
1. Pathogenesis of ulcerative colitis bleeding
Up to now, although the pathogenesis of CAP is not really clear, the most mentioned hypothesis is that the pathological condition is caused by many factors that combine to create including genetic, environmental, Intestinal microbiota leads to inappropriate inflammatory responses.
Identified mechanisms include:
A: Disturbances of the gut microbiota with depletion of beneficial bacterial strains, especially Firmicutes and Bacteroidetes leading to invasion through the mucus layer of microorganisms harmful bacteria. B: increased expression of the Toll-like receptor TLR-4 C: Accumulation of mucin-containing glycosylated precursors leads to poor quality of intestinal mucus secretion (impaired barrier) D: CD10 antigen-carrying dendritic cells release TL27 that activate differentiated immature CD4 T cells and natural killer cells. CD4 T cells differentiate into Regulatory T and Helper Breathing T cells that further produce eosinophil activators. Activated natural killer cells produce IL-13, which destroys epithelial cells, changes the function of the intercellular junction, causes fibrosis, and IL-23, which activates Th7 cells. IL17 production, thereby inducing neutrophil chemotaxis. E: Activation of B-cells that produce antibody words The association between genetic factors and the onset and progression of CAP has not been demonstrated as clearly as in Crohn's. However, studies in identical and fraternal twins have shown that the incidence of this disorder is also 16% in identical twins and 2% in fraternal twins. To date, 47 gene sites have been identified related to CF, of which 20 overlap with Crohn's such as: IL-10, IL-23, Janus-kinase-related pathway, etc. . . In addition, a number of gene sites specific for CKD have been discovered such as hepatocyte nuclear factor-4a, cadherin 1, laminin-B1 that play a role in leukocyte mobilization, change binding of epithelial cells thereby weakening the cell's protective barrier.
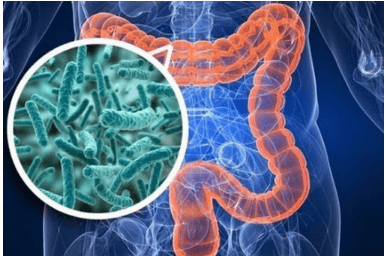
2. Intestinal microbiota
Gut microbiota is fully established in the first few months postpartum and is fairly stable throughout life, although there may be times when there may be some variation. It is estimated that there are about 15,000 - 36,000 bacterial strains that make up the intestinal microbiota, of which the most abundant strains are Firmicutes and Bacteroidetes. Under normal physiological conditions, intestinal bacteria play an important role in the maturation of intestinal mucosal cells, keeping balance, nutrition, protection and repair of mucosal lesions.
In IBD pathologies, many studies have shown that in intestinal mucosa biopsies, the number of bacteria is much higher than in healthy people, but the diversity of bacterial strains is significantly reduced. since, from 30 - 50% and there is a difference between Crohn's and CKD. The strains identified as beneficial to the body such as Bacteroidetes and Firmicutes (especially Eubacterium and Lactobacillus) were significantly reduced while the number of pathogenic strains such as E.coli increased. These changes play an important role in IBD, but it is controversial whether this is a cause or effect of the mucositis process.
A study compared the changes of intestinal microbiota in areas of colonic mucosa with lesions and areas of healthy mucosa in patients with active RA. The results show that there is no difference in the microbiota in the two mucosal regions, which helps to suggest the hypothesis that the change in the intestinal microbiota plays a primary role, contributing to a reasonable pathogenesis. than.
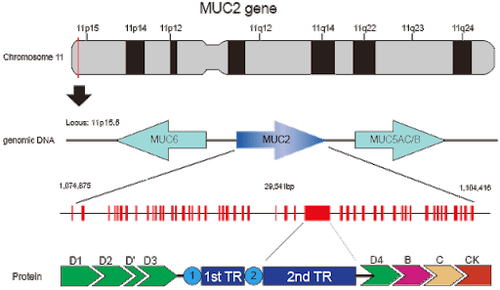
3. Intestinal barrier
The intestinal mucosa is covered with a protective mucus layer that helps to avoid direct contact of pathogenic factors. Mucus is composed of protein, carbohydrate, and lipid components, of which the main component is the mucin glycoprotein encoded by the MUC2 gene. Mucus is formed into the endoplasmic reticulum of goblet cells and Paneth cells, then glycosylated in the Golgi system, sulphated, and released out of the cell as granules containing mucin complexes. Besides, mucus also contains many substances with anti-bacterial properties such as defensin, cathelicidin, lysozyme produced from Paneth cells and enterocytes, trefoil peptide released with MUC2 from goblet cells. A number of studies have demonstrated that in the active phase of CAP, there is a decrease in the thickness of the mucus layer, a decrease in the number of goblet cells, an increase in neutrophil infiltration and direct contact of the submucosal layer with other pathogens. intestinal bacteria. When the protective barrier in the epithelial layer is broken, the permeability of the cell membrane will change, resulting in the affected intercellular junction. This phenomenon leads to increased exposure to antigens leading to activation of innate and acquired immune system responses.
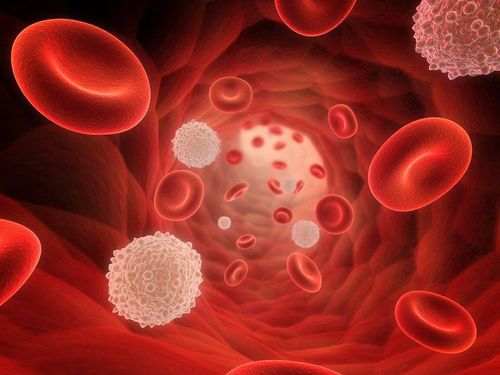
4. Cells involved in the pathogenesis of CKD
Currently identified cells involved in the pathogenesis of CAP include:
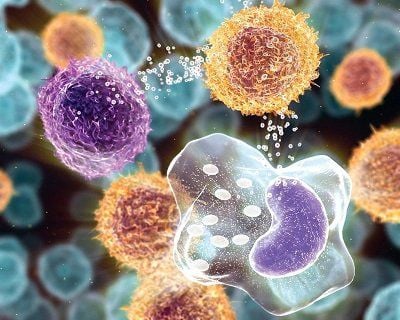
4.1 Antigen presenting cells Antigen presentation to these cells in the gut is the first step in the activation of the antigens. inflammatory cytokines. Dendritic cells have recognition receptors called PRRs (pattern-recoginition receptors) that are able to respond to antigens inside and outside the cell. When the permeability of the epithelial barrier is altered, antigens can penetrate the connective membrane and activate dendritic cells. Microbial lipopolysaccharides can activate dendritic cell maturation. Dendritic cells, after being recognized and activated, will release IL-12, which affects the maturation of the original T cells into cell walls. In addition, the activation of dendritic cells also produces many inflammatory cytokines and chemokines that cause neutrophils to accumulate and activate other immune cells. Macrophages located in the gastrointestinal mucosa are locally activated when antigens are present. This process leads to the release of a variety of proinflammatory factors such as TNF-4, IL-1, IL-6, IL-8, IL-12, IL-18, IL-23. In addition, macrophages secrete active metabolites of oxygen and nitrogen, proteases capable of degrading extracellular structures. Thus, macrophages play an important role in the progression of inflammation as well as in the remission phase when intestinal mucosal lesions are restored.
4.2 Helper T-cells Pathogenesis is related to the acquired immune system because antigen-presenting by dendritic cells leads to the release of cytokines with cell activation and differentiation effects T.
T cells can be differentiated into regulatory or active T cells. An imbalance between T-cell lines leads to inflammation. Helpers are cells that play a role in generating immune responses, which are divided into two groups of Thi and Th2. In the past, the authors thought that the immune response in RA is through Th2, but recent studies show that the immune response of this disease is not really Th2 because of the upregulation of IL-13. ,IFN-Y and no IL-4 involvement.
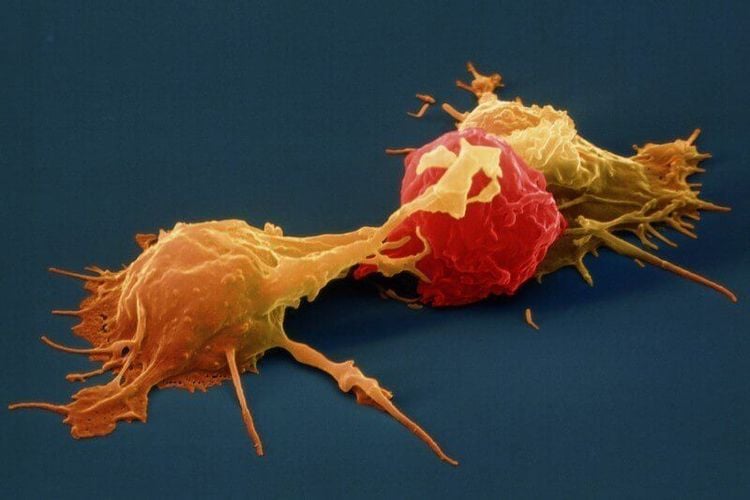
4.3 Natural killer cells Natural killer cells are natural killer (NK) imprinted T cells that are capable of producing both Thi (IEN-1) and Th2 (IL-5, IL) cytokines -13). When glycolipid antigens are presented to a natural killer cell, which destroys epithelial cells, forming ulcers while IL-13 induces apoptosis of epithelial cells. In addition, JL-13 also has the effect of enhancing the cytotoxicity against natural killer cells.
5. Cytokines
These are transducer signals that play a role in enhancing and maintaining the specific immune response in CKD. Besides the common host cytokines such as TNF-2, IL-1, IL-6, other cytokines produced by Th2 cells such as IL-10, IL-13 also play a certain role.
6. Proinflammatory cytokines
TNF-a plays a role in activating inflammation, producing IL-1B, IL-6, fibroblast differentiation, activating coagulation factor precursors and initiating an acute response from which to initiate. initiation of programmed cell death.
TNF-a also activates macrophages, lymphocytes, and B cells and stimulates T cells to increase pro-Y production as well as initiating the (NF)-KB pathway that plays a role in differentiation, growth, and differentiation. cell wall and control of proinflammatory cytokines. Therefore, increased production of TNF- will induce inflammatory lesions in the intestinal mucosal barrier of CKD patients.
IL-1 is produced by macrophages and plays a proinflammatory-like regulatory role in the pathogenesis of CAP. JL-1 consists of IL-la and IL-10 that help in the production of cyclooxygenase type 2, nitric oxide synthase and phospholipaseA. An IL-1 receptor antagonist (IL-1Ra) is responsible for controlling inflammation. In CKD patients, IL1-Ra levels are elevated and the higher the IL-1Ra/IL-1 ratio, the more severe the disease activity. In addition, in IBD patients, increased levels of IL-1B in the colonic mucosa have been reported.
Several other factors have also been found to play a role in the pathogenesis of the disease, as high levels of IL-6 found in serum and tissues are associated with clinical severity. This is explained by the fact that IL-6 binds to the slL-6R receptor, creating a complex that stimulates cells to express the cell surface protein gp130. When this protein is activated, STAT3 will also be activated, leading to an effect on a number of cells in the cell, creating factors that resist apoptosis (Bcl-2, Bcl-xL). T cells that are resistant to apoptosis play a role in promoting chronic inflammation.
IL-9 is produced from Th9 cells that are matured under the influence of TGF-B and IL-4. IL-9 affects the intestinal mucosal barrier barrier through regulation of Claudin-2, a major mediator of intestinal barrier drainage. Several studies have shown that there is an overexpression of IL-9 in biopsies of inflammatory tissues in patients with SLE and that increased serum IL-9 levels correlate with the severity of the patients.
IL-13 is a Th2-specific cytokine produced by natural killer cells and plays a role in destroying the intestinal epithelial cell layer, IL-13 changes the permeability of the intestinal mucosa and the junction. epithelial cells. In addition, this factor also impairs the repair process of mucosal damage.
IL-33 is a new pro-inflammatory factor that acts as an "alarm" for the immune system in the gut. IL-33 is produced from damaged intestinal mucosal epithelial cells and induces immune responses. The IL-33 receptor is present on the surface of Th2 and I-regulatory immune cells, and also on Thi. The first studies on this proinflammatory factor in patients with RA showed that, whether in stable or active disease, IL-33 levels were higher than in normal subjects [35, 36]. Then another study demonstrated that after anti-TNF treatment, the expression of IL-33 was significantly reduced compared with the acute phase.
7. Anti-inflammatory cytokines
TGF-8 is an anti-inflammatory cytokine responsible for regulating and maintaining the balance between inflammatory and immune responses. This factor helps the mucosal healing process and protects the mucosa from changes in the gastrointestinal tract in ACS [38]. IL-10 is produced from B cells, cells and monocytes, which inhibit the production of TNF-α, IL-1B and IL-6. Therefore, IL-10 is often elevated in CKD patients while in normal people, this factor has a very low concentration, undetectable. Mutational loss of function 4 of the IL-10 receptor 4 has been shown to be associated with severity in patients with ACS.
8. Some other cytokines
Typically, IL-8 plays a role in chemotaxis of polymorphonuclear leukocytes to the gastrointestinal tract wall, IL-8 is produced by many types of cells such as T cells, endothelial cells, fibroblasts but mainly monocytes and macrophages. This cytokine is highly expressed in the damaged mucosal areas, thereby attracting many inflammatory cells, especially polymorphonuclear leukocytes, to concentrate here. This helps to suggest a mechanism for acute inflammatory injury and possibly the formation of microabscesses in the intestinal mucosa in IBD.
The pathogenesis of hemorrhagic ulcerative colitis is quite complicated and until now there is no cure for this disease completely. Patients are often recommended to maintain a good diet for the digestive system, avoid stress and have regular health checkups.
Currently, the Department of Gastroenterology - Vinmec International General Hospital constantly updates the modern equipment and machinery with a team of expert doctors to help endoscopy diagnose stomach and colon diseases such as inflammation, ulcers, polyps, cancer, finding HP bacteria, detecting cancer early in the digestive tract... are accurate, thereby providing a good treatment for each patient's health condition.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
NagreF, Gionchetti PR, Eliakim R. et al. (2017). Third European Evidence-based consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and lleo- anal Pouch Disorders. J Crohn's Colitis, 11(6), 649-670. De Dombal F.T. (1968), Ulcerative colitis: definition, historical background, aetiology, diagnosis, naturel history and local complications, Postgrad Med J,44(515), 684-692. Crohn's B.B. (1962). An historic note on ulcerative colitis. Gastroenterology, 42, 366-367. Lichtenstein G.R., btv. (2014), Medical Therapy of Ulcerative Colitis, Springer-Verlag, New York.