This is an automatically translated article.
Corticosteroids are adrenal hormones with important physiological roles, including regulation of glucose metabolism, protein catabolism, alteration of calcium metabolism, regulation of bone turnover, suppression of the immune system, and downregulation of inflammatory process. Because of their diverse effects, corticosteroids have been used in the treatment of respiratory diseases such as asthma, chronic obstructive pulmonary disease, idiopathic pneumothorax, and infectious disorders.
1. What are corticosteroids?
Corticosteroids are anti-inflammatory drugs, similar to cortisone, a hormone produced in the body by the adrenal glands. Cortisone is needed by the body to fight injury, infection, and other diseases.Corticosteroids are very different from anabolic steroids used by some athletes to improve muscle mass and performance. Corticosteroids are used to treat respiratory conditions and are used to help control a variety of inflammations. For example, they can be used to treat inflammation of the intestines (colitis), in the joints (arthritis), in the skin (dermatitis), and in the lungs (asthma and other lung disorders). Corticosteroids are sometimes used in higher doses to suppress the immune system, such as to help prevent rejection of a transplanted organ.
Asthma is caused by inflammation of the airways, the main lung condition for which corticosteroids are used. They can also sometimes be helpful in chronic obstructive pulmonary disease (COPD), which includes chronic bronchitis and emphysema.
Anti-inflammatory corticosteroids are also useful in the treatment of other lung diseases, such as sarcoidosis and long-term inflammatory conditions (alveoli).
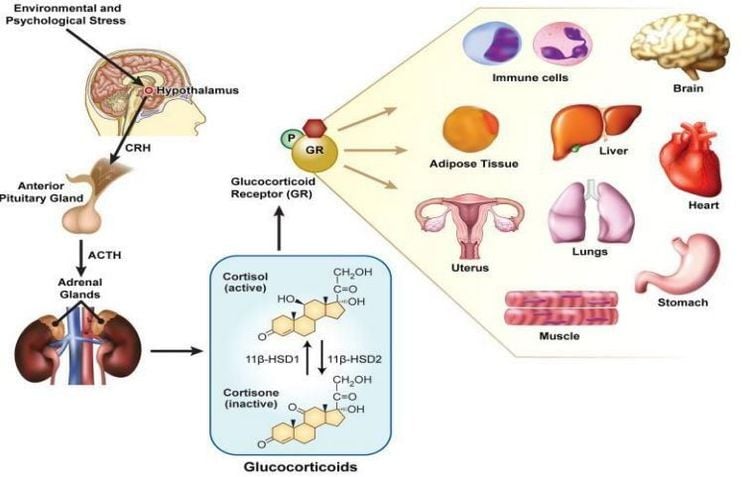
2. Physiological effects of Corticosteroids
Corticosteroids play an important physiological role in the human body and are called “stress hormones”. One of the most important effects of corticosteroids is their ability to regulate glucose synthesis. Glycogen is the main storage form of glucose in humans and is stored in various organs of the body, especially the liver. Glycogen is a multi-branched polysaccharide and its structure consists of a core protein (glycogenin), which gives rise to many branches consisting of glucose monomers. Glycogen is produced by a biochemical pathway known as glycogenesis, which mainly occurs in the liver. Glycogen is broken down during fasting to provide glucose monomers. Glucose monomers can be used by all cells of the body through glycolysis.
Pyruvate generated during glycolysis can then produce acetyl-CoA which can enter the Krebs cycle. The oxidation of glucose (in combination with the electron transport chain) produces adenosine 1,4,5-triphosphate (ATP), which is the cell's energy currency.
Stress hormones (such as catecholamines) normally regulate gluconeogenesis and glycogenolysis to cause hyperglycemia, helping to meet the energy needs of various cells in the body. Corticosteroids also induce fasting hyperglycemia by upregulating gluconeogenes, which is achieved by increasing the expression of several important enzymes involved in gluconeogenesis, including phosphoenol pyruvate-carboxykinase, fructose-1, 6-bisphosphatase and glucose-6-phosphatase.
Cortisol and other corticosteroids are special in that they regulate gluconeogenesis while inhibiting glycogenolysis. This seemingly contradictory effect of corticosteroids is important for survival in utero as the release of cortisol from the fetal adrenal glands helps build glycogen stores in the fetal liver in preparation for delivery.
Protein metabolism is also affected by corticosteroids. Increased catabolism of proteins to amino acids provides a source of alanine, which can be converted to glucose by gluconeogenesis. The Cahill cycle (glucose-alanine cycle) refers to a series of chemical reactions in which amino groups and carbon skeletons from muscles are transported to the liver as alanine, which is then converted to glucose. An enzyme required for the Cahill cycle is alanine aminotransferase (ALT), which is present in both muscle and liver. Alanine aminotransferase (also known as serum glutamate-pyruvate transaminase [SGPT]) is responsible for converting an amino group from alanine to α-ketoglutarate, resulting in the production of pyruvate and glutamate. Pyridoxal phosphate is a cofactor for this reaction and is formed from pyridoxine (vitamin B6). As Corticosteroids regulate protein catabolism, they cause a negative nitrogen balance in the body, which is important during times of starvation.
Corticosteroid giúp điều trị bệnh hô hấp và kiểm soát nhiều chứng viêm khác nhau.
Some other effects are also caused by corticosteroids, not evident in the physiological state. However, in disease states, these actions can lead to protean manifestations. Corticosteroids are required for optimal functioning of the body and an excess or deficiency of these hormones can manifest as Cushing's syndrome or Addison's disease. Cushing's syndrome is most commonly hormonal and results from exogenous steroid use, although it can also result from tumors that secrete cortisol or adrenocorticotropic hormone (ACTH), such as pituitary adenoma, adrenal adenoma or carcinoma, small cell carcinoma of the lung, etc.).
Common features of this disease are obesity, lipodystrophy, lunar facies, purple ventral striae, easy bruising, depression, psychosis, cataracts, glaucoma, hypertension, hypokalemia and hypocalcemia. On the other hand, Addison's disease can be caused by an autoimmune destruction of the adrenal glands (in developed countries) or by an infection such as tuberculosis (in developing countries) entering the adrenal gland. Hypokalemia manifested by asthenia, fatigue, weight loss, hyperpigmentation (due to increased ACTH secretion from the pituitary gland), hyponatremia, hyperkalemia, orthostatic or resting hypotension, hypercalcemia blood, basophils, or eosinophils. Treatment of these diseases is aimed at restoring the balance of steroid hormones back to normal. In the case of Cushing's syndrome, where the underlying cause is resolved (eg, removal of the primary tumor), rarely bilateral adnexectomy with exogenous steroid replacement may be required. In Addison's disease, steroid hormone replacement is often needed. These two diseases demonstrate the importance of corticosteroids and the harmful consequences of their excess or lack of them on the human body.
3. How are corticosteroids used in the treatment of respiratory diseases?
In the treatment of respiratory diseases, Corticosteroids can be taken by mouth (tablets), injected, inhaled with an inhaler, nebulizer or dry powder device.
Corticosteroids taken by mouth are called oral corticosteroids. Predni Solone (Solone, Panafcortelone, Prednisolone) is the most commonly used oral corticosteroid. Other examples include dexamethasone (Dexamethasone) and cortisone acetate (Cortate).
Inhaled corticosteroids include:
Fluticasone (in Flixotide, Seretide, Breo). Budesonide (in Pulmicort, Symbicort). Beclomethasone (in Qvar). Ciclesonide (in Alvesco). They are preferred in the treatment of respiratory diseases, such as asthma and COPD because of their direct impact on the airways. Inhaled medicine reaches the small airways in the lungs to be effective, and this requires the correct use of the inhaler. Your doctor or pharmacist can advise you on the correct method to use.

Corticosteroid giúp điều trị bệnh hô hấp được bác sĩ sử dụng theo đúng phác đồ
4. How do corticosteroids work?
The most important effect of corticosteroids is to reduce inflammation. Inflammation within the lining of the bronchial tubes in the lungs is a major cause of asthma symptoms. Regular daily use of inhaled corticosteroids is very effective for preventing asthma symptoms and flare-ups.
Inflammation is also present in the lungs of people with COPD, where it causes swelling and narrowing of the airways, increasing mucus. Inhaled corticosteroids can be used as a regular daily treatment to help prevent flare-ups in people with severe COPD or frequent flare-ups.
5. When are oral corticosteroids used?
Prednisolone is usually used for short periods of asthma or COPD flare-ups, when there is a sudden worsening of symptoms.
In severe asthma or COPD that is difficult to control with inhaled therapy, lower doses of prednisolone may be used long-term.
Oral corticosteroids are sometimes used in other lung diseases. Corticosteroids used in this way are usually only given for a few days to a few weeks. In some long-term inflammatory conditions of the lungs (eg, alveolitis or sarcoidosis) they may be needed for longer periods of time. Your doctor will advise you on effective methods.
6. What are the side effects of oral corticosteroids?
Corticosteroid side effects are more common when they are taken for a long time and in high doses. However, they can still occur at lower doses and for short periods of time in some people. With proper care and planning, many side effects can be predicted or reduced.
With oral corticosteroids such as prednisolone, longer-term side effects include weight gain, increased susceptibility to infections, delayed healing, easy bruising, osteoporosis and growth retardation in children. To reduce the risk of fractures, your doctor may prescribe medications to help keep your bones strong.
In some people, corticosteroids can raise blood sugar and make diabetes more difficult to treat. This may lead to a change in the dose of your diabetes medication.
The development of side effects can also depend on the disease for which the corticosteroid is prescribed, for example a low dose in rheumatoid arthritis can produce side effects, whereas, the same dose amounts in sarcoidosis may not cause any side effects.
Sometimes oral corticosteroids can affect mood and many people feel happier during treatment. On the other hand, some people may experience depressed mood.
Corticosteroids can reduce the healing of the stomach lining, leading to bleeding from the front of the ulcer. You should tell your doctor if you have ever had a peptic ulcer, indigestion or heart burn. In this situation, your doctor may prescribe a medication that helps protect the stomach.
A rare but serious side effect is hip damage when taking high doses of oral corticosteroids for a long time. If you have any concerns about possible side effects, report them to your doctor as soon as possible.

Bên cạnh tác dụng điều trị bệnh hô hấp, Corticoid có thể gây tình trạng bầm tím.
7. What are the side effects of inhaled corticosteroids?
Inhaled corticosteroids are preferred over oral corticosteroids because less doses are needed and are delivered directly to the lungs. This means there are fewer side effects when using inhaled corticosteroids.
The most common side effects are hoarseness and sore throat. A sore throat can be caused by a fungal infection (thrush) or by propellant in the blisters. Rinsing, rinsing, and spitting up after each dose and use of a spacer will help avoid these problems.
High doses of inhaled corticosteroids can contribute to osteoporosis and may also increase blood sugar levels in some people. Your doctor may choose to check your bone density or blood sugar if this is a concern. Some people with COPD who use high doses may also have an increased risk of pneumonia.
8. Are there other precautions?
When oral corticosteroids are used for longer periods of time, they can decrease the body's production from the adrenal glands. It is important not to stop using oral corticosteroids suddenly or without consulting your doctor. This is because it can take weeks or months for the adrenal glands to start producing cortisone in the normal way again. Therefore, always buy medicine on time so that you do not run out of medicine.
In a nutshell, Corticosteroids are anti-inflammatory drugs, similar to cortisone, a hormone produced in the body by the adrenal glands. Cortisone is needed by the body to fight injury, infection, and respiratory diseases.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.