This is an automatically translated article.
Article by Doctor Vu Duy Dung - Department of General Internal Medicine - Vinmec Times City International General HospitalEvaluate a patient who has had a seizure that is different in many respects from a patient with a first seizure. In particular, the chances of getting reliable information from an eyewitness to the seizure are higher, and the ability of the EEG to catch epileptic abnormalities is also increased. In patients with multiple recurrent seizures, video EEG may be considered, and brain imaging should focus on structural abnormalities that warrant surgery.
1. Seizure Assessment
Patients who already have epilepsy may have multiple seizure patterns. Inquiry should guide patients to describe seizures in their own words, to identify the different seizure patterns associated with specific epilepsy syndromes, or to recognize that seizures Localization usually develops from a prodromal to loss of consciousness and sometimes convulsions. There are many sources of eyewitness information that can be gathered, and the patient or family may have recorded the episode on video. It may also be clear to family members and other bystanders that the patient is not aware of some seizures. For patients with epilepsy who continue to have seizures, we wanted to know if seizures were caused by some factor, either non-adherence to medication or an indicator of an incomplete drug response that required correction. drug or not. Seizures can be experienced at most times of the day or be triggered by specific circumstances, suggesting a rare form of reflex epilepsy.
Physicians need to use a systematic amount of descriptive vocabulary to capture the key components of a clinical seizure and its progression. Many epilepsy centers use this lexicon to create a seizure classification based solely on clinical symptoms and observed behavioral signs, useful for localizing the site of seizure onset. and capture all the key components of a seizure and its progression. Such test independence allows the description of a seizure without knowing the pattern of onset on the EEG, which is often more practical.

Một số triệu chứng lâm sàng của bệnh động kinh có thể quan sát được
The International League Against Epilepsy (ILAE) seizure classification was revised in 2017. The terms for each seizure type indicate suspected or confirmed (localized) EEG onset. with the whole), followed by a brief description of the patient's symptoms, creating an electro-clinical entity. The concise version separates partial cognitive seizures and focal impairment seizures. Partial and generalized seizures can be classified as motor and nonmotor. A longer version allows for a more detailed description.
Approximately 70% to 80% of patients with chronic partial epilepsy will also develop epileptic discharges in addition to the seizure. Values are noticeably higher in chronic partial seizures than in first-time seizures. Capability to capture projectiles depends on recording time. Today, most patients and physicians prefer the convenience of an ambulatory EEG and its ability to be read by a specialist who reads repeated routine EEGs. In a study by Faulkner et al., in epileptic patients who had an abnormal epileptic pattern within 4 days of EEG recording, epileptic discharges were observed in 44% of patients within 4 hours. , 58% within 8 hours, 85% within 24 hours, and 95% within 48 hours of recording. A full 96-hour recording detects only 5% of extraepileptic epileptic discharges. Mean latency to first discharge was significantly shorter in patients with generalized epilepsy (43 min) than in partial seizures (512 min with extratemporal epilepsy and 590 min with temporal lobe epilepsy). ), shows that a log length of 2 days is mostly sufficient to find epileptic activity in addition to seizures and a log length may be shorter in cases of suspected generalized epilepsy.
In most patients, especially if they respond to medical therapy and are seizure-free, a determination of seizure type and seizure type through symptomatology and extra-epileptic EEG is sufficient to manage. However, in patients whose seizures are still resistant after 1 year, an evaluation in the epilepsy monitoring unit is recommended to determine the actual cause of the seizures. Approximately 25% of patients considered treatment-resistant are found to have non-epileptic attacks, and 10% to 20% of patients with epilepsy also have non-epileptic attacks. Some patients with generalized epilepsy will not be recognized unless they are monitored drug-free for several days. Last but not least, there are a significant number of patients with partial epilepsy who are candidates for epilepsy surgery who would benefit from a preoperative evaluation in the epilepsy monitoring unit.
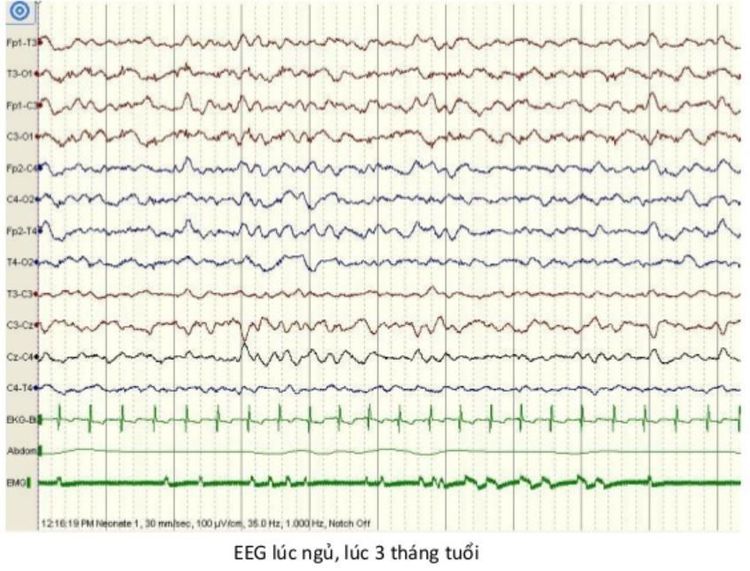
Hình ảnh kết quả EEG lúc ngủ của trẻ 3 tháng tuổi
2. Electro-clinical syndromes sorted by age of onset Neonatal
Benign familial neonatal epilepsy Premature myoclonic encephalopathy Ohtahara syndrome
Infants
Infantile epilepsy with moving partial seizures West syndrome Infant myoclonic epilepsy Benign infantile epilepsy Benign familial infantile epilepsy Dravet syndrome Encephalopathy myoclonus in non-progressive disorders Infants
Febrile seizures plus (may begin in infancy) Panayiotopoulos syndrome Seizures with atonic (previous) myoclonic seizures auto-limited epilepsy with central-temporal spikes autosomal dominant nocturnal frontal lobe epilepsy Late-onset infantile occipital lobe epilepsy (Gastaut body) Seizures with myoclonic absence seizures Lennox-Gastaut syndrome Disease cerebral epileptic seizures with continuous spike-waves in sleep Landau-Kleffner syndrome Childhood absence seizures Juvenile to adult
Juvenile absence seizures Juvenile myoclonic seizures Seizures with tonic-clonic seizures- Isolated generalized seizures Progressive myoclonic epilepsy Autosomal dominant epileptic seizures with symptoms Auditory symptoms Other familial temporal lobe epilepsy Not particularly related to age
Familial partial seizures with variable foci (infancy to adulthood) Reflex seizures
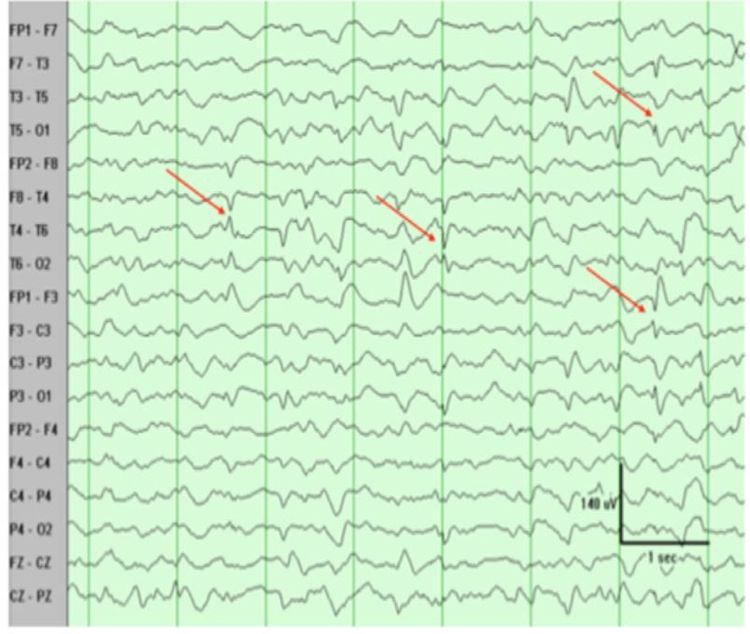
Hội chứng Lennox-Gastaut trên hoạt động nền thường xuất hiện sóng chậm, có thể cả sóng nhọn 2 pha, 3 pha.
3. Epilepsy The next step in the evaluation is to determine the type of epilepsy: partial, total, or unknown. In the ILAE classification, seizure types and epilepsy types greatly overlap; however, there is an acknowledged subgroup of patients (eg, patients with Lennox-Gastaut syndrome or Dravet syndrome) who may have focal and generalized onset seizures and presentation with a combination of generalized and partial epilepsy. In partial seizures, the epilepsy type should be further subdivided according to the anatomical region of the suspected seizure source based on epileptic description, imaging, and out-of-crunch EEG, or identified by episodes recorded by video EEG during the seizure. and accordingly classified as temporal, frontal, or parietal, left or right epilepsy.
4. Epilepsy Syndromes Many different epileptic syndromes have been described, many with onset in childhood or adolescence. Recognizing these syndromes is not only important for treatment and prognosis, but also guides genetic testing because many of the identified epileptic syndromes are likely to have genetic causes.
Source:
Stephan US. Evaluation of Seizure Etiology From Routine Testing to Genetic Evaluation. Continuum (Minneap Minn) 2019;25(2, Epilepsy):322–342
Please follow the series of articles on "Evaluating seizure causes from routine tests to genetic testing" by Dr. Vu Duy Dung including:
Part 1: Evaluation of epilepsy causes from tests routine referral to genetic testing Part 2: New-onset seizures Part 3: Epileptic assessment Part 4: Extra-genetic causes of epilepsy Part 5: Genetic causes of epilepsy