This is an automatically translated article.
Papillary thyroid nodules are the most common type of thyroid cancer. The disease is sometimes only discovered when papillary thyroid cancer has metastasized, has spread beyond the thyroid gland and the prognosis is often difficult.1. What is papillary thyroid nodule?
Papillary thyroid carcinoma, also known as papillary carcinoma, is the most well-differentiated form of thyroid cancer. At the same time, this is also the most common form of thyroid cancer with the main cause being exposure to radiation energy.This type of thyroid tumor usually presents as irregular nodules or cysts or as tumors in the normal thyroid parenchyma. Once advanced, papillary carcinoma can be minimally invasive or overly invasive. In fact, these tumors can easily spread to other organs, invade the lymphatic system, but are less likely to invade blood vessels.
Fine-needle aspiration biopsy is always considered the first and best diagnostic procedure in all cases when a nodule or a nodule is found in the thyroid gland. At this time, radical surgery will be indicated for definitive intervention and management if it is papillary thyroid cancer. Approximately 4-6 weeks after thyroidectomy, the patient may receive adjuvant radioactive iodine therapy to detect and destroy any remaining metastatic cells and malignant tissue in the thyroid gland.
The prognosis of patients with papillary thyroid nodules is also related to age. Future outcomes are better in younger patients than in patients older than 45 years.

U tuyến giáp thể nhú hay còn gọi là ung thư biểu mô nhú, là một dạng ung thư tuyến giáp biệt hóa tốt nhất
2. What are the causes of papillary thyroid nodules?
The thyroid gland is a parenchyma that is particularly sensitive to the effects of various types of ionizing radiation. Both incidental and medical exposure to ionizing radiation are associated with an increased risk of thyroid cancer.Accordingly, with radiation therapy measures have been used to treat many malignant tumors and benign lesions, such as treating acne or excessive facial hair growth, tuberculosis in the neck, scalp fungus, thymectomy, tonsils, these patients will later be at risk of developing thyroid cancer for up to 30 years. Furthermore, patients who receive radiation therapy for certain types of head and neck cancer, especially during childhood, may have an increased risk of developing thyroid cancer.
In addition, some epidemiological studies have shown other causes of papillary thyroid nodules as follows:
Dietary iodine deficiency Use of oral contraceptives Presence of nodules Benign thyroid gland Late menopause Late childbirth Uncommon familial syndromes such as adrenal polyps, Gardner's syndrome, and Cowden's disease may be associated with thyroid papillomas in about 5% of cases.
3. What is the pathological progression of papillary thyroid nodules?

Biểu hiện ban đầu phổ biến nhất của u tuyến giáp thể nhú là một nốt sần có thể cảm thấy ở cổ
The most common initial presentation of a papillary thyroid nodule is a palpable nodule in the neck. Therefore, for any patient with a recent and emerging thyroid nodule, a thorough medical history should be taken by the physician to identify any associated symptoms or risk factors. mandarin. In particular, special attention is paid to the exposure to ionizing radiation and the duration of radiation. At the same time, a family history of thyroid cancer should also be noted. In addition, some patients with thyroid cancer have persistent cough, difficulty breathing, or difficulty swallowing. Pain is rarely an early warning sign of thyroid cancer. Other symptoms such as vocal cord paralysis and hemoptysis are rare.
At the time of diagnosis, about 10-15% of patients with papillary thyroid cancer have distant metastases to the bones and lungs. Meanwhile, these patients were initially misdiagnosed with local diseases of the lungs or bones, such as lung tumors, bone tumors or pathological fractures.
3.2 Examination
The clinician examines the thyroid gland by palpating the patient's neck to assess the size and density of the thyroid gland. At the same time, the presence of any nodules or nodules in the thyroid gland should also be noted.
The main sign of papillary thyroid nodule is a palpable nodule, usually solitary in the thyroid region, and has the following features:
Painless Has a solid density Average size less than 5 cm Boundary unspecified Fixed to surrounding tissue Moves with trachea when swallowing If papillary thyroid nodule has metastasized, lymph nodes in the neck may be palpable on one or both sides. In addition, some patients also have a feeling of tightness or fullness in the neck, hoarseness or signs of compression of the trachea or esophagus.
3.3 Disease progression
Papillary thyroid neoplasms represent only a small percentage of all adult cancers. However, in women, thyroid cancer is the fifth most common cancer. Of all thyroid cancers, most are papillary thyroid neoplasms and the incidence is higher in areas where goiter is common.
Prognosis in patients with papillary thyroid tumors is related to age, sex, and stage. Prognosis is better in women and in patients younger than 40 years of age. As well, the survival rate is at least 95% with appropriate treatments. In contrast to many other cancers, papillary thyroid nodules are mostly curable. The reason is that thanks to the slow progression of the disease, the prognosis is relatively positive. The median 10-year survival rate is higher than 90%, and distant metastases, i.e., malignant cells reaching the lungs or bones, are rare.
However, if the disease is detected when thyroid cancer has caused symptoms due to compression or invasion of the cancerous tumor into surrounding tissues, in order of frequency it is the lungs, bones, brain, liver and other organs. Otherwise, the prognosis has become dire.
4. Diagnostic methods for papillary thyroid nodules

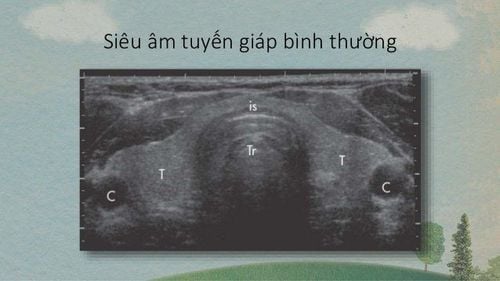
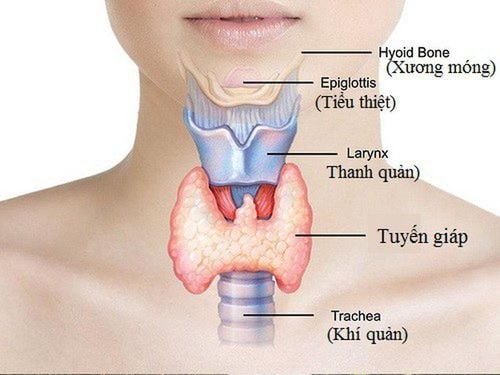
Siêu âm tuyến giáp là một trong số những phương pháp để chấn đoán u tuyến giáp
Thyroid function tests Thyroid tests thyroid stimulating hormone (TSH) Serum carcinoembryonic antigen (CEA) levels (reference range <3 ng/dL). Thyroid ultrasonography Fine needle biopsy for pathology is the “gold standard” Imaging tools by chest X-ray, computed tomography and magnetic resonance imaging to assess distant metastases. In summary, the most common type of thyroid cancer is papillary thyroid nodule. The disease has a good prognosis if it is detected early and treated radically from the beginning. Therefore, when an abnormal thyroid nodule is discovered by chance, it is necessary to visit a thyroid specialist early and make a diagnosis and determine the nature of the lesion to rule out the possibility of malignancy.
Currently, Vinmec International General Hospital has a package of screening and screening for thyroid diseases. When choosing the Package of Screening and Screening for Thyroid Diseases at Vinmec, you will be examined by experienced thyroid specialists to help screen and detect common thyroid diseases early. variables such as: simple goiter, hyperthyroidism, hypothyroidism, thyroiditis, thyroid nodules, thyroid cancer,...
At the same time, you will have blood tests, evaluate levels of functional hormones thyroid such as FT3, FT4, TSH, Anti - TPO, Anti TG and ultrasound, scan to evaluate the structure of the thyroid gland. After that, when the results are returned to the doctor, you will be consulted about thyroid pathology, and discuss the appropriate treatment options for yourself. From there, thyroid disease will be prevented in time, avoiding long-term health damage in the future.
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE
SEE MORE
Benign thyroid nodules need surgery? TSH hormone and its significance in the diagnosis and screening of thyroid diseases Where is the thyroid gland located and what function does it have?