This is an automatically translated article.
Posted by Master, Doctor Hoang Duc Nam - Department of General Surgery - Vinmec International General HospitalPancreatic duct stones are the result of chronic pancreatitis, they are also the cause of recurrent acute pancreatitis, or aggravation of pain associated with chronic pancreatitis due to obstruction and increased pressure in the pancreatic duct.
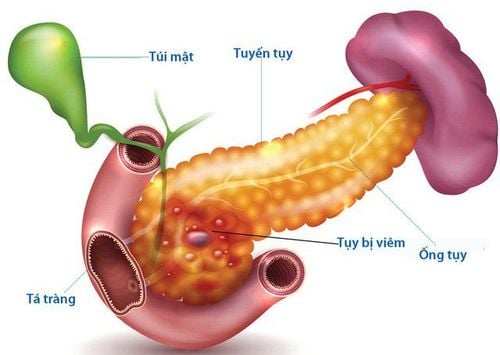
1.Overview of chronic pancreatitis The pancreas is an organ in the abdomen, normally the pancreas performs an exocrine function by producing digestive enzymes (amylase, lipase) and then secreting it into a duct called a duct. pancreas, emptying into the first part of the small intestine (duodenum) to aid in the digestion of food (fat, protein..)
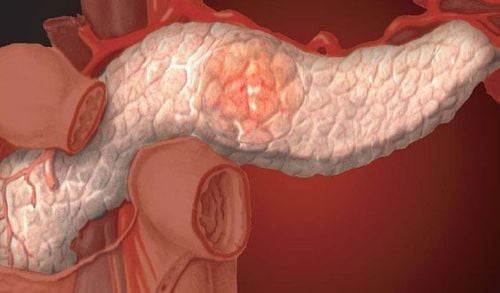
Chronic pancreatitis occurs when the pancreas is damaged by recurrent inflammation for a long time. Inflammatory changes affect the normal functioning of the pancreas. Patients with chronic pancreatitis often require ongoing medical care to minimize symptoms, slow damage to the pancreas, and manage possible complications.
Most chronic pancreatitis presents with pancreatic duct stones, so the names are almost identical for these two concepts.
While pancreatic duct stones are the result of chronic pancreatitis, they are also the cause of recurrent acute pancreatitis, or aggravation of pain associated with chronic pancreatitis, by obstructing and increasing intraductal pressure. pancreas.
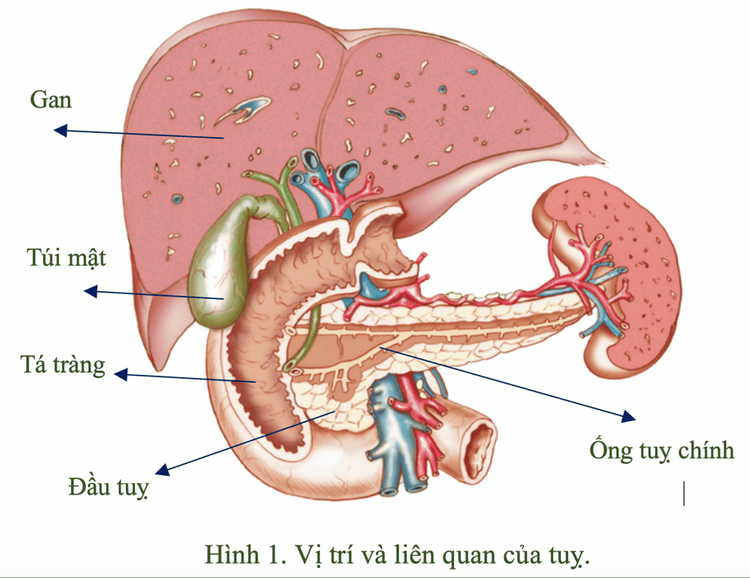
Hầu hết viêm tụy mạn biểu hiện bởi sỏi ống tụy
2. Causes and risk factors for pancreatitis
The most common causes of chronic pancreatitis include:
Alcohol abuse (most common) Hereditary pancreatitis Obstruction of the pancreatic duct (due to trauma, stuck stones, tumor insertion..) Certain diseases other (such as lupus) Cystic fibrosis or a cystic fibrosis gene mutation Too high levels of triglycerides (a form of blood fat)
3. Manifestations of chronic pancreatitis/pancreatic stones
Most commonly, mid-abdominal pain is dull and persistent, there may also be episodes of more severe abdominal pain if acute inflammation is present. Patients with chronic pancreatitis often have difficulty digesting fat in food; lead to weight loss and frequent diarrhea. In more severe cases, the pancreas loses its ability to produce insulin, leading to diabetes.
Abdominal pain: Usually occurs in the abdomen above the navel, pain spreads to the back, relieves pain by sitting upright or bending forward; may be accompanied by nausea and vomiting. Pain usually worsens about 15-30 minutes after eating. However, about 20% of people with chronic pancreatitis have no pain at all.
Impaired pancreatic function: Normally, the pancreas helps digest food and control blood sugar levels. In people with chronic pancreatitis, pancreatic function is not guaranteed to be maintained, leading to limited digestion and absorption of fat in the gastrointestinal tract. Thereby causing the manifestation of raw feces and scum, with an unusual smell. This symptom usually does not occur, until 90% of the damaged pancreatic tissue loses its function.

Người bệnh xuất hiện triệu chứng đau bụng phần trên rốn và lan ra sau lưng
4. Complications of pancreatitis
Chronic pancreatitis can lead to various complications, including:
Obstruction of the common biliary and pancreatic ducts, leading to obstructive jaundice and exacerbations of acute pancreatitis. Obstruction at the beginning of the digestive tract (not able to eat, slow digestion in the upper abdomen...) Increases the risk of pancreatic cancer
5. Diagnosis of chronic pancreatitis/pancreatic stones
The diagnosis of chronic pancreatitis can be difficult; Signs and symptoms are nonspecific and can be similar to those found in many other digestive conditions, such as peptic ulcer disease, gallstone disease, irritable bowel syndrome, or even pancreatic cancer.
Tests may be normal, especially during the first two or three years of illness. Sometimes it is also difficult to distinguish chronic pancreatitis from acute pancreatitis (more sudden..).
Blood test : Can detect digestive enzymes that escape from the pancreatic duct and increase in the blood when the pancreas is inflamed. Stool test: Record high or low levels of pancreatic elastase in the stool. Imaging: Unprepared X-ray may show contrast-enhanced stones in the pancreatic duct; Ultrasound-computerized tomography and abdominal magnetic resonance imaging help evaluate the structure of the pancreas, the condition of the pancreatic ducts and bile as well as the adjacent tissues around the pancreas. With endoscopic retrograde cholangiopancreatography or endoscopic ultrasonography, it helps to evaluate the pancreatic ducts as well as the surrounding tissues. This test involves inserting an endoscope from the mouth into the first part of the gastrointestinal tract, up to the junction of the bile duct.
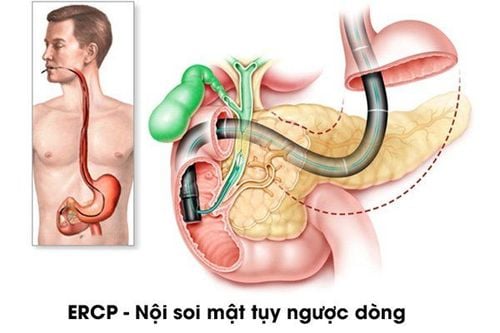
Kỹ thuật nội soi mật tuy ngược dòng được sử dụng trong chẩn đoán viêm tụy mạn/sỏi tụy
6. Treatment of chronic pancreatitis/Pancreatic stones
The treatment of chronic pancreatitis is to help relieve pain, improve pancreatic function as well as manage complications.
Pain relief: Many interventions are aimed at providing pain relief for patients with chronic pancreatitis. Simple measures can be effective in the early stages of the disease; while at a later stage the treatment can be much more complicated.
Avoid alcohol: Is the MOST IMPORTANT treatment in cases of pancreatitis associated with alcohol abuse. The results may help reduce chronic pancreatitis pain and reduce the risk of pancreatitis exacerbations. Stop smoking: Also improves pain in chronic pancreatitis. Low-fat diet: Eating small meals and drinking enough water can improve the pain of chronic pancreatitis. Fasting for several days with parenteral replacement fluids (in a hospital setting) also helps relieve persistent pain in pancreatitis. Pain relievers: In the early stages of the disease, simple pain relievers can also be effective, such as ibuprofen. Pancreatic enzyme supplements: To provide and replace the normal pancreatic enzymes that must be produced, helping the pancreas to "rest". However, pancreatic enzymes are not effective in alleviating pain in all cases. Nerve blocker: Injection of drugs destroys nerve tissue that transmits sensation from the pancreas. Helps to improve chronic pain in 50% of cases, often requires repeat procedures and also has many risks that need to be discussed more carefully with the patient. Nerve blockade is therefore only applicable to patients who experience severe pain due to chronic pancreatitis - who have not responded to other analgesics.

Hình ảnh ống thông đặt từ mũi đi vào qua thực quản, dạ dày và tá tràng, đi vào trong ống tụy. Ở phía ngoài, đầu ống được nối vào 1 quả bóp giúp hút dịch tụy ra và theo dõi lưu lượng hàng ngày. Với phương pháp này hầu hết bệnh nhân ra về an toàn. So với nội soi đặt ống thông (stent) bên trong có thể gặp tắc stent hoặc nhiễm trùng tại chỗ thì phương pháp này ưu việt hơn.
Endoscopy (from the stomach) dilates the pancreatic duct (with the part that shares the bile duct) - to reduce pressure inside the tube, can improve pain sensation. After dilation, a cannula (metal or plastic) can be placed in place or a catheter is inserted through the nostril.
Endoscopy: Aims to reduce elevated pressure in the lumen of the pancreatic duct caused by a stone blockage, which may improve pain in some patients.
Pancreatic lithotripsy : Pancreatic stones are usually trapped behind a narrow spot in the pancreatic duct and usually require surgical resection of the underlying sphincter and dilation of the stricture to pull the stone out. Extracorporeal lithotripsy can be used to break up stones that are stuck or large into smaller pieces, which can be pulled out. The technique is successfully performed in 60% of cases, complications can be encountered in 20%. 70% of patients showed marked improvement in symptoms after the intervention. Surgery: Usually reserved for patients who do not respond to other analgesia and have dilated pancreatic ducts. There are two commonly used surgical methods:
Decompression surgery : Perform anastomosis of the main pancreatic duct with the first part of the small intestine, after removing the large pancreatic stones and stones blocking the blockage. The appendage of the intestine acts as a bridge to carry the pancreatic juice that has just been secreted down the digestive tract, reducing the pressure in the lumen of the pancreatic duct. This method is effective in 80% of patients. Removal of the head of the pancreas : It is believed to be the main cause of obstruction of the pancreatic duct and later bile duct; It is also the place where pain is given. The results of resolution as well as prevention of biliary obstruction as well as pain relief, although not all cases are sustained pain management.
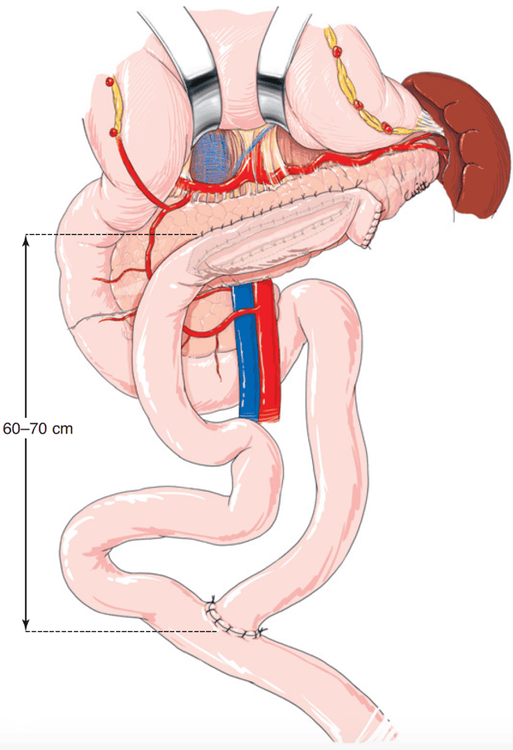
Phẫu thuật giảm áp ống tụy (Nối ống tụy-hỗng tràng)
Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit examination and treatment at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References: emedicine.medscape.com, uptodate.com, Aussilhou B, Cherif R, Dokmak S, Sauvanet A. Dérivation chirurgicale du canal de Wirsung dans la pancréatite chronique. EMC - Techniques chirurgicales - Appareil digestif 2016;11(2):1-14 [Article 40-881].