This is an automatically translated article.
The article was written by Dr. Dao Thi Mai Lan - Medical Specialist - Gene Technology, Vinmec Stem Cell Research Institute and Gene Technology.
Atrial fibrillation is common in the elderly. It is estimated that one in 10 people over the age of 80 has atrial fibrillation. Different types of heart disease, such as valvular heart disease, heart attack, or heart failure, can also cause atrial fibrillation. Any type of infection that causes inflammation of the myocardium or the outer layer of the heart can lead to atrial fibrillation.
1. What is atrial fibrillation?
Arrhythmias are disorders that affect the normal heart rhythm when the heart tends to beat too slow (bradycardia), too fast (tachycardia) or irregularly.
Atrial fibrillation is a heart rhythm disorder or irregular heartbeat that occurs when electrical signals in the heart are disrupted. Different types of atrial fibrillation can last for a few seconds or be permanent. This condition is more common in older adults and can have many different causes. Many people with atrial fibrillation lead perfectly normal lives, but atrial fibrillation also increases the risk of stroke.
Normally, the heart's pumping action is controlled by electrical impulses. The electrical impulse starts at the sinoatrial (SA) node and then propagates throughout both atria causing both atria to contract, forcing blood into the ventricles. The electrical impulse then travels down the atrioventricular (AV) node from here splitting into two branches, allowing the electrical signal to propagate evenly to both ventricles at the same time.
Next, both ventricles contract to push the blood out. When the heart is working normally, this cycle repeats 50 to 150 times per minute. With atrial fibrillation, electrical impulses begin to travel from both atria in an irregular fashion with so many random triggers that the heart beats irregularly and sometimes too quickly.
There are different types of atrial fibrillation:
Paroxysmal AF: atrial fibrillation that comes and goes in episodes. Attacks can last a few seconds or up to a few days, but usually, attacks start and go away on their own. Persistent AF: Episodes of atrial fibrillation that last for more than a week and will not stop if left untreated. Persistent atrial fibrillation: The heart is always in a state of atrial fibrillation. Despite trying a number of different types of treatment, there was no way to get the heart rate back to normal. Atrial flutter: Atrial flutter is a state in which the atria beat too quickly. Atrial flutter is similar to atrial fibrillation but less common. Many patients have both atrial flutter and atrial fibrillation. In fact, the treatments for both are similar, and the stroke risk for both is the same.

2. Causes of atrial fibrillation
Some people are born with heart problems that may develop atrial fibrillation later in life. Other health conditions such as high blood pressure, diabetes, sleep apnea, or lung disease can also increase your risk of atrial fibrillation. In many cases, people with atrial fibrillation have no known cause.
3. Possible complications of atrial fibrillation
If left untreated, atrial fibrillation can lead to an increased risk of serious problems such as stroke or heart failure.
Stroke : Because the atria can't push blood properly, blood gets trapped in the small corners and grooves of the heart. When trapped, the blood can clot. With all the abnormal contractions in the atria, these clots can be pumped into the circulatory system. If a blood clot reaches the brain, it can block a blood vessel leading to a stroke. Sometimes, blood clots can also travel to other parts of the body and cause other complications. >>> Atrial fibrillation and stroke risk
Heart failure: If atrial fibrillation is not controlled early, it can lead to heart failure. This happens when the heart has to work too hard to keep blood circulating throughout the body. As a result, excess fluid builds up causing swelling in the ankles and legs or it can build up in the lungs leading to shortness of breath and fatigue. Other complications: For some people, atrial fibrillation can cause fatigue, weakness, or shortness of breath. Uncontrolled atrial fibrillation can also cause chest pain, dizziness, and fatigue. In the elderly, it can cause episodes of confusion. Although not life-threatening, these symptoms can limit a person's daily activities and quality of life.

4. Symptoms
Symptoms of atrial fibrillation include:
Fast heartbeat or feeling that the heart rate is "skipped" Shortness of breath Dizziness or feeling faint Fatigue or lack of energy Chest pain, tightness Anxiety or feeling not OK These are the most common symptoms. The person may feel only one or a few of the above symptoms or may have other symptoms. Many people have no symptoms. In fact, many people with atrial fibrillation are able to keep their symptoms to a minimum and have a normal quality of life.
5. Diagnosis of atrial fibrillation
To diagnose atrial fibrillation, your doctor will review your medical history, conduct a complete physical exam, and order some tests. Some common tests ordered include:
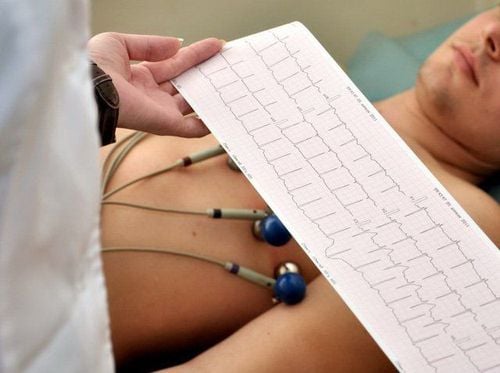
Electrocardiogram (ECG): This test records the electrical activity of the heart to confirm if the heart rhythm is accompanied by atrial fibrillation. Holter Monitor : The device records the electrocardiogram continuously for up to 48 hours. This is a small portable device that you can carry with you during your ECG. >>> What is Holter electrocardiogram and what does it mean in the diagnosis of arrhythmia?
Event recorder: Similar to the Holter, an event recorder is a portable device worn outside the body that records heart activity for up to two weeks. Patients can press the "record" button whenever they feel abnormal, such as a fast heartbeat, dizziness or chest pain. Echocardiogram: Ultrasound imaging allows the doctor to see the heart chambers and heart valves. >>> Types of echocardiography at Vinmec
6. Treatment
Atrial fibrillation is not usually life-threatening, but it still needs to be treated because it can affect a person's quality of life. Atrial fibrillation slows the flow of blood through the heart, increasing the chance of blood pooling and forming blood clots. If a blood clot enters the circulation, it can block an artery and lead to a stroke.
Drug treatment: Medications to relieve symptoms help control heart rate, slow heart rate to help the heart return to a normal rhythm. The choice of a treatment plan will depend on a number of factors including: The type of atrial fibrillation you have, other heart or health problems, and your symptoms.
Reduce the risk of stroke with anticoagulants: To prevent blood from clotting in the heart anticoagulants (blood thinners) may be used. Anticoagulants do not actually thin the blood, rather, they increase the time it takes for a clot to form. The type of anticoagulant a patient takes will depend on other medical conditions, along with overall stroke risk. Anticoagulants are very effective in reducing the risk of stroke and are recommended for almost all people with atrial fibrillation.
The most common procedures for treating atrial fibrillation are electrical cardioversion and catheter ablation.
Electrical cardioversion : This procedure involves delivering a shock to the heart like a defibrillator with only a smaller amount of electricity. Electrical cardioversion is only a short-term solution. In most patients, atrial fibrillation will return. Catheter ablation: This procedure involves threading a thin wire through a vein in the groin or neck. The tip of the catheter points towards the areas in the heart that are emitting abnormal impulses. Once in place, the catheter will deliver a small radiofrequency current to ignite at the identified location.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














