This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.Oddi dysfunction is a rare clinical entity that is often forgotten in the typical distinction. Although the course of Oddi dysfunction is not inherently dangerous, effective treatment can improve a patient's quality of life.
1. What is a sphincter disorder?
Sphincter of Oddi dysfunction is a rare clinical entity. When determined to significantly improve the patient's quality of life. As a diagnosis of exclusion, the typical patient will present with recurrent biliary colic, usually after undergoing cholecystectomy in association with inflammation, pancreatitis, or both.
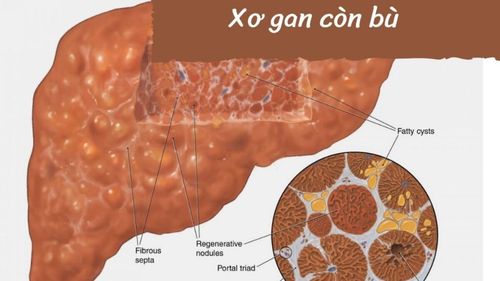
More severe cases may progress to clinically apparent obstructive jaundice and chronic pancreatitis, although rare. Some of these signs and symptoms are also present in more severe disease processes, but once ruled out, attention should be directed to Sphincter of Oddi dysfunction as a possible cause of patient difficulty. bear.
2. Pathophysiology of Oddi . dysfunction
The exact cause of Oddi dysfunction is unclear. The concept of this disease process is easier when one understands that sphincter of Oddi dysfunction is a broad term that describes a wide range of hepatobiliary disorders. These clinical entities result from a variety of sphincter dysfunction, including inappropriate spasm, tightening, or relaxation. Furthermore, this disease process may involve the biliary sphincter, the pancreas, or both. The clinical sequelae reflect the pathogenesis of these organ systems.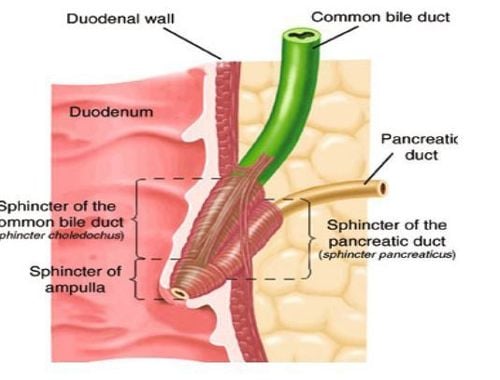
Epidemiologically, Oddi dysfunction occurs most frequently in women between the ages of 20 and 50. Prevalence is about 1.5% but this is likely an underestimate as it has not been tested. and lack of specific biochemical markers for identification. In individuals with recurrent idiopathic pancreatitis and chronic pancreatitis, the prevalence of sphincter of Oddi dysfunction can be as high as 72% and 59%, respectively. Therefore, sphincter of Oddi dysfunction must be much higher than reported.
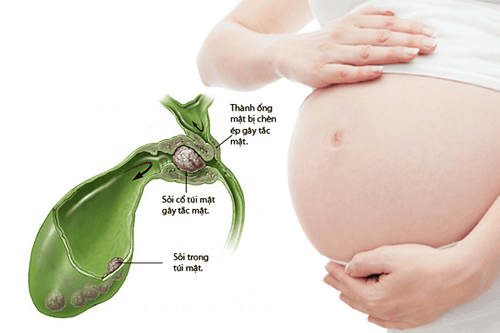
Risk factors for developing multiple sphincter of Oddi dysfunction include prior cholecystectomy and lithotripsy, gallbladder degeneration, biliary tract stones, liver transplantation, alcohol use disorders, hypothyroidism and irritable bowel syndrome (IBS). While the list is quite varied, in each context it is conceivable that an influence on the pancreatic system could affect sphincter function or bile flow.
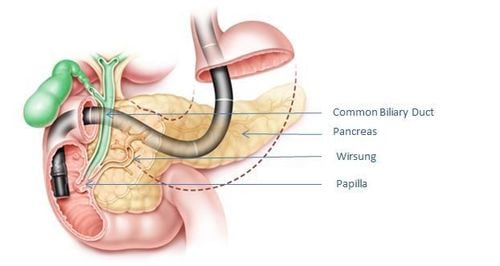
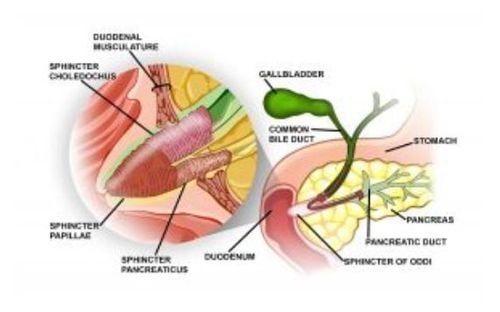
3. Pathophysiology of Oddi dysfunction The sphincter of Oddi has three main functions, which are to regulate the flow of bile into the duodenum, prevent reflux into the bile duct or pancreas, and promote gallbladder filling. between digestive cycles.
Baseline sphincter pressure is 10 mmHg, with intermittent phase increases in tone from 2 to 6 times per minute and from 50 to 140 mmHg. Cholecystokinin (CCK) has been shown to relax basal tone and inhibit physical contractions. Cholecystokinin, released from endocrine cells in response to a meal, has a direct hormonal effect on the sphincter. Other gastrointestinal peptides have different effects on the sphincter, these include gastrin, secrettin, motilin, and octreotide. In addition, there is extrinsic control of the sphincter through sympathetic innervation.
As mentioned above, Oddi dysfunction often presents with recurrent biliary colic symptoms. Both sphincter stenosis and dyskinesia can be telltale signs of symptoms.
4. Clinical Manifestations Most patients presenting with sphincter of Oddi dysfunction will complain of biliary pain. Their discomfort was mainly located in the epigastrium as well as the right upper quadrant, with radiation reaching the back and shoulders. It usually lasts about 30 minutes to several hours before disappearing spontaneously. This pain may be accompanied by nausea and vomiting.
In contrast to biliary colic, symptoms are not usually postprandial, unless the primary source of sphincter dysfunction involves the pancreatic ductal component of the sphincter. Recurrent or chronic pancreatitis can also be a sign of underlying sphincter dysfunction.
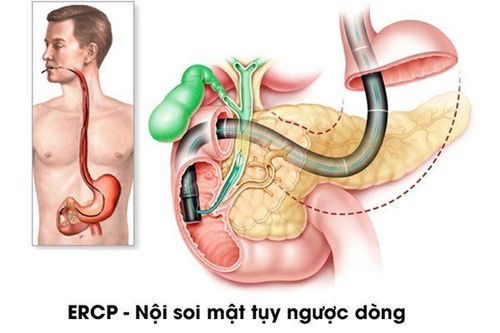
Endoscopic retrograde cholangiopancreatography (ERCP) with manometry is considered the gold standard test for the sphincter of Oddi dysfunction. A sphincter pressure above 35 to 40 mmHg on manometer is consistent with the diagnosis of sphincter of Oddi dysfunction. Importantly, however, even this modality may overlook patients with clinically apparent sphincter of Oddi dysfunction. For types I, II and III, the frequency of abnormal sphincter of Oddi manometer is 85.7%, respectively; 55.1% and 28.1%. Thus, even with the most clinically evident (class I) patient, approximately 15% of people fail to demonstrate the expected pressure, suggesting that isolated sphincter pressure measurements may not be accurate. adequately assess a disease process whose symptoms are of an intermittent nature. Therefore, although ERCP with manometer is the gold standard, it should be considered along with other measures.
Laboratory evaluation should also be performed, in particular, a comprehensive metabolic panel (CMP), amylase and lipase to evaluate for hepatopancreatic dysfunction. Functional testing, such as the Nardi test, can also help confirm the diagnosis. The Nardi test involves the simultaneous use of morphine and neostigmine.
Patient presentation combined with examination results is used to classify the sphincter of Oddi dysfunction. Specific diagnostic criteria for sphincter of Oddi dysfunction include:
Elevated liver enzymes (2 times the upper limit of normal) Common bile duct dilation (greater than 10 mm on ultrasound; greater than 12 mm for ERCP) biliary colic-type pain Using these criteria, patients were classified as follows:
Type I sphincter of Oddi dysfunction: All three criteria above Oddi sphincter dysfunction type II: Pain of biliary origin (biliary colic) and one of the other two criteria. Sphincter of Oddi dysfunction type II: biliary colic-type pain. The results of this classification will influence subsequent treatment plans.
6. Treatment and management of Oddi dysfunction The treatment of Oddi sphincter dysfunction is aimed at reducing basal pressure and valve resistance in the sphincter of Oddi. Noninvasive options include calcium channel blockers, tricyclic antidepressants, glyceryl trinitrate, and somatostatin, each with varying degrees of success.
For example, in a randomized controlled trial, nifedipine was shown to reduce cumulative pain scores and symptom episodes, emergency department visits, and analgesic consumption compared with placebo medicine. However, the combination of the aforementioned therapies showed an even greater degree of symptom relief. One study using a combination of nifedipine, a tricyclic antidepressant, and glyceryl trinitrate, found that 15.3% and 59.3% of patients reported that symptoms resolved or improved completely.
Invasive interventions to treat Oddi dysfunction include ERCP and sphincterotomy. This modality has been shown to be highly effective and safe for the patient.
Injecting botulinum toxin into the sphincter has been shown to reduce sphincter tone by approximately 50%, but has not resolved the patient's symptoms in a small series of cases. However, botulinum toxin and stenting have both been suggested as interim steps to clarify whether sphincter relaxation/stent placement resolves symptoms, thereby providing a means of predicting response. of patients towards more definitive sphincterotomy.
Patients with sphincter dysfunction type I and type II of Oddi dysfunction should be referred for management with ERCP and sphincterotomy. Type III sphincter dysfunction was demonstrated in a trial that did not respond to procedural intervention. Instead, these patients should be referred for medical management, including pain management.
7. Differential diagnosis Oddi dysfunction is often considered a diagnosis of exclusion. The difference between epigastric pain and right lower quadrant pain is very broad. Therefore, it is important to perform appropriate testing to rule out other disease processes before formally diagnosing and treating sphincter of Oddi dysfunction. The spectrum of obstructive cholangiopathy, including gallstones and malignancies such as cholangiocarcinoma, requires specific attention. These must especially be considered if bile duct dilation and transaminase elevations are present.
Although the course of Oddi dysfunction is not inherently dangerous, effective treatment can improve a patient's quality of life. All patients with suspected sphincter of Oddi dysfunction can be treated with ERCP and sphincterotomy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Jordan P. Crittenden; Jeffery B. Dattilo. Sphincter of Oddi Dysfunction. Treasure Island (FL): StatPearls Publishing; 2021 Jan-(https://www.ncbi.nlm.nih.gov/books/NBK557871/)