This is an automatically translated article.
Ocrelizumab is used to treat some forms of primary progressive or relapsing multiple sclerosis (MS). The drug comes in the form of an injectable solution and is usually injected into a vein as prescribed by your doctor.1. What does Ocrelizumab do?
Ocrelizumab is used to treat some forms of primary progressive or relapsing multiple sclerosis (MS). However, because of its nature as a monoclonal antibody, Ocrelizumab cannot completely treat multiple sclerosis. But Ocrelizumab can reduce the number of relapses and prevent (or delay) possible disability.2. How to use Ocrelizumab Before taking the drug, patients need to follow these important instructions:
Ocrelizumab is a solution, which is injected into the patient's vein by a doctor or nurse. Ocrelizumab is usually given every 2 weeks for the first two doses (at week 0 and week 2), then once every 6 months. Ocrelizumab can cause very serious (rarely fatal) side effects called infusion reactions during or up to 24 hours after treatment. Your doctor or nurse will monitor your reaction during the injection and for at least 1 hour afterward. Tell your doctor or nurse if you notice any of these side effects: rash, itching, trouble breathing, swelling, sore throat, tiredness, fever, fainting, flushing, nausea, aches headache, dizziness, heart palpitations. You may also be given extra medication before each dose, including corticosteroids (such as Methylprednisolone), antihistamines (such as Diphenhydramine), and Acetaminophen to help reduce the severity of the injection.
3. Undesirable effects of the drug Ocrelizumab
Some unwanted effects that may occur during taking the drug can be listed as:Like many other drugs, Ocrelizumab can also bring some side effects such as: cold symptoms such as cold symptoms such as: stuffy, runny nose or cough. Ocrelizumab may decrease your ability to fight infections. It can even make you more susceptible to serious (but rarely fatal) infections or make any existing infections worse. Tell your doctor right away if you have any signs of infection (such as sore throat or persistent cough, fever, chills, cold sores on the lips or genitals, shingles). . Before prescribing this medication, your doctor will do a blood test to check if you are infected with hepatitis B. If you have had hepatitis B in the past, Ocrelizumab can cause the condition to return and lead to serious liver problems. In rare cases, Ocrelizumab may increase your risk of developing cancer, including breast cancer. Tell your doctor right away if you have symptoms such as abnormal breast growth or nipple discharge.
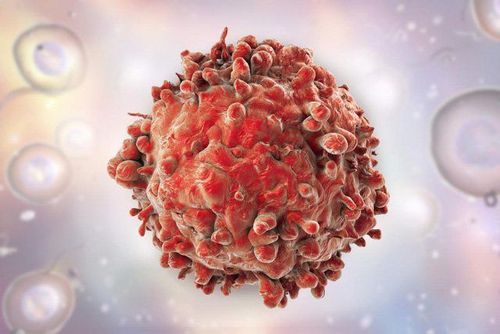
Ocrelizumab có thể làm tăng nguy cơ phát triển ung thư
Ocrelizumab may increase your risk of a rare but very serious (possibly fatal) brain infection called progressive multifocal encephalopathy (PML). Get medical help right away if you experience any of these new or more serious side effects: clumsiness, loss of coordination, balance, weakness, confusion, trouble concentrating, dementia memory loss, seizures, difficulty speaking, vision changes.
4. Be careful when using Ocrelizumab
Before taking Ocrelizumab medicine, keep a few things in mind:If you are allergic to the active ingredient Ocrelizumab or have any other conditions, tell your doctor right away. Tell your doctor about your medical history, especially: past or present infections (including hepatitis B, herpes, tuberculosis), life-threatening infusion reactions to ocrelizumab . Ocrelizumab may make you more susceptible to infections or may worsen any existing infections. Avoid contact with people with contagious infections such as chickenpox, measles, and flu. Do not get vaccinated unless approved by your doctor. Avoid contact with people who have recently received a live vaccine (such as the flu vaccine inhaled through the nose). Tell your doctor if you are pregnant or plan to become pregnant. You should not inject Ocrelizumab during pregnancy because it can harm an unborn baby. It is advisable to actively use reliable methods of contraception while taking the drug and for 6 months after stopping treatment. If you accidentally become pregnant, talk to your doctor right away about the risks and benefits of this medication. Newborns born to mothers receiving Ocrelizumab should be tested for vaccine responsiveness before any vaccine is given. It is not known whether Ocrelizumab passes into breast milk. If you are taking this medicine for multiple sclerosis consult your doctor before breast-feeding. Some drugs that can interact with Ocrelizumab are: drugs that weaken the immune system, increase the risk of infection such as Natalizumab, Rituximab. If you overdose on Ocrelizumab and you notice symptoms such as fainting or shortness of breath, you need to take the patient to the emergency room immediately. Medical tests (such as blood tests to check for Hepatitis B, breast cancer screening, Immunoglobulin levels) should be done before you start using this medicine, as well as during and after treatment. It is important to get your injections on schedule. If you accidentally miss a dose, ask your doctor or pharmacist right away for a new injection schedule.

Thuốc Ocrelizumab cần dùng theo chỉ định và hướng dẫn của bác sĩ
Above are the uses of Ocrelizumab and explain what Ocrelizumab does? In order for the use of the drug to be highly effective, patients need to know the information and it is necessary to consult with doctors and pharmacists before taking it.
Vinmec International General Hospital has a team of doctors and pharmacists with many years of experience. Therefore, when there are any health problems or questions about the use of drugs, customers can contact the hospital for examination and appropriate indications.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: Webmd.com