This is an automatically translated article.
Post by Master, Doctor Mai Vien Phuong - Gastrointestinal Endoscopy - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.In patients who are obese and have advanced chronic liver disease or end-stage nonalcoholic steatohepatitis, assessment of eligibility for liver transplantation should be conducted in a timely manner. Once a patient undergoes orthopedic liver transplantation, metabolic comorbidities should be closely monitored and adequately treated.
1. Overview
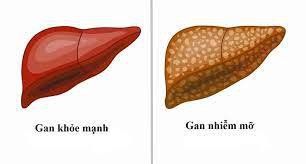
With obesity, metabolic dysfunction-associated fatty liver disease/nonalcoholic steatohepatitis, the management of patients with chronic liver disease becomes quite complex. Patients with metabolic dysfunction-associated steatohepatitis/nonalcoholic steatohepatitis are more likely to have multiple diseases, exhibit different features of the metabolic syndrome, and increase the risk of morbidity and mortality due to metabolic syndrome. Heart.In the early stages of liver disease without evidence of cirrhosis (fatty liver disease associated with metabolic dysfunction), management of comorbidities will guide therapy, while in As patients develop nonalcoholic steatohepatitis and liver fibrosis, liver-related complications as well as mortality become relevant.
2. Obesity and fatty liver disease associated with transfer dysfunction before and after liver transplantation
In general, patients with cirrhosis/end-stage liver disease should be managed according to existing guidelines for the treatment of portal hypertension, because of the mortality associated with end-stage liver disease, especially those with obese patients. According to the U.S. Organ Transplantation Network/Organ Transplant Registry Liver Transplant Report, 36.9% of adult patients undergoing liver transplantation were obese [BMI (30 kg/m2)] including 14 .8% with a BMI of more than 35 (kg/m2). Despite the caveat that BMI is not an ideal parameter in patients with end-stage liver disease due to ascites, these data still highlight obesity as an important comorbidity in transplantation. liver.
3. Obese patients are no longer considered a contraindication to liver transplantation Due to the increasing experience of treating these patients, obesity [BMI (40 kg/m2)] is no longer considered. is contraindicated for liver transplantation. However, specific challenges include technical difficulty during surgery, as well as a higher incidence of morbidity in the postoperative period, especially due to an increased risk of infection. Ultimately, these challenges lead to increased 30-day mortality.
Regarding the long-term outcomes of liver transplant recipients of nonalcoholic steatohepatitis, survival rates are comparable with other causes. Despite the fact that Malik et al found an alarming 1-year mortality rate of 50% in patients with nonalcoholic steatohepatitis, obesity ≥60 years of age with type 2 diabetes, hypertension arterial pressure. Therefore, pre-transplantation should ensure an extensive benefit-risk assessment on a case-by-case basis before a liver transplant is indicated to avoid unwanted complications
4. Weight gain after liver transplantation After liver transplantation, weight gain is common, regardless of the underlying chronic liver disease and the type of organ transplanted. Overall, about one in three liver transplant recipients becomes overweight or obese within 3 years. Decreased physical activity, energy excess intake as well as older age are beneficial for the development of obesity, increased risk of cardiovascular disease and metabolic disorders.
Although a clear program of studies was launched in 2014 by the American Society for Transplantation, outcome measures were heterogeneous and liver transplant recipients were underrepresented in studies this. A recent review of 2 observational and 3 randomized controlled trials by Dunn et al reported that exercise intervention groups often performed better in endurance tests, energy expenditure amounts at metabolic equivalents and peak or peak oxygen uptake.
An even recently published prospective study reported that financial incentives resulted in more patients achieving their goal of >7000 steps per day, however, this did not translate to little weight gain. than. Another study using a smartphone app found that 35% of participants had a significant increase in their physical performance, but did not report whether this translated into an outcome benefit. Thus, despite a positive effect on surrogate parameters, there is little or no high-quality evidence on whether exercise has a direct effect on overall survival or outcome. liver involvement after transplantation or not.
In terms of outcome parameters, BMI was significantly lower in spine surgery patients 2 years after liver transplantation, with significantly lower rates of arterial hypertension and diabetes. Note, however, that prospective randomized studies are needed to compare whether the benefits outweigh the risks in terms of overall outcomes, which presents some difficulty in establishing this.
6. Dyslipidemia in the post-liver transplant stage In addition to weight gain, the rate of dyslipidemia is high in the post-transplant stage and affects about 40%-70%. In part, dyslipidemia and impaired glucose tolerance are metabolic side effects of immunosuppressants such as calcineurin inhibitors, the mammalian target of rapamycin and corticosteroid inhibitors. Therefore, statins are commonly used after liver transplantation, but data regarding statin therapy and its potential effects on portal pressure and hepatocyte function in post-transplant conditions are scarce and unavailable. clear guidelines for the use of statins after transplantation. However, it has been shown that dyslipidemia is associated with increased morbidity and mortality in liver transplant recipients.
Recently, a study by Patelet demonstrated good statin tolerance and survival benefit in patients on statin therapy after liver transplantation, supporting the use of statins in this setting as well. Furthermore, experimental studies in rats have demonstrated the graft-protective effect of statins when added to cryopreservation. Overall, limited, high-quality prospective studies are lacking, but available evidence suggests a beneficial effect of statins in post-liver transplantation conditions.
7. Post-liver transplant insulin sensitivity issues Although glycogen synthesis is improved, only a few patients show an improvement in insulin sensitivity after liver transplantation. In contrast, 10 to 30% of patients with new-onset type 2 diabetes after liver transplantation are associated with corticosteroid and tacrolimus use. In the immediate post-transplant period, insulin is considered the safest and most effective option for antihyperglycaemic treatment. However, for the management of persistent type 2 diabetes after liver transplantation, evidence is scarce.
A recent meta-analysis stated that safety and efficacy for various anti-hyperglycaemic agents in the post-transplant setting cannot be concluded, as the studies are currently of insufficient quality. High. Therefore, antihyperglycemic therapy after first-line metformin should be selected according to patient preference and clinical features, such as the presence of chronic kidney disease, heart failure, or obesity.
8. Current challenges in the treatment of metabolically-associated fatty liver disease Metabolic-associated fatty liver disease (non-alcoholic steatohepatitis) is a complex disease entity, placing presents challenges to clinical practice and requires interdisciplinary management for optimal patient care. In recent years, several new concepts have been established and bariatric surgery has proven to be an effective treatment option. In addition, recent trial results suggest that new treatments or alternative medicines may be effective for ameliorating fatty liver disease associated with metabolic dysfunction or achieving weight loss. sustainable and potentially ameliorate secondary metabolic disorder-associated fatty liver disease. Therefore, the multifactorial nature of the disease and the interconnectedness of different aspects requires up-to-date knowledge, especially as more treatments are available.
9. Adherence is of primary importance These developments require an individualized treatment plan and must be based on patient preferences, as adherence is of primary importance. In patients with advanced chronic liver disease or end-stage nonalcoholic steatohepatitis, assessment of eligibility for liver transplantation should be conducted in a timely manner. Once a patient undergoes orthopedic liver transplantation, metabolic comorbidities should be closely monitored and adequately treated. In the future, the unique metabolic vulnerability of liver transplant patients will become even more relevant, as nonalcoholic steatohepatitis as a marker for liver transplantation is rapidly increasing, underscoring the importance of liver transplantation. importance of future trials in this particular group of patients. In summary, obesity has led to a significant increase in patients with metabolic dysfunction-associated fatty liver disease (MAFLD). While dyslipidemia, type 2 diabetes, and cardiovascular diseases guide treatment in patients without evidence of liver fibrosis, morbidity and mortality become associated with the progressive form of infectious liver disease. steatosis, nonalcoholic steatohepatitis (NASH), and development of cirrhosis.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References:
Hartl L, Elias J, Prager G, Reiberger T, Unger LW. Individualized treatment options for patients with non-cirrhotic and cirrhotic liver disease. World J Gastroenterol 2021; 27(19): 2281-2298 [DOI: 10.3748/wjg.v27.i19.2281]
Cotter TG , Charlton M. Nonalcoholic steatohepatitis after liver transplantation. Liver transplant. Year 2020; 26: 141-159. [ PubMed ] [ DOI ] [ Citation in this article : 3 ] [ Citation in CrossRef: 6 ] Eslam M , Sanyal AJ, George J; International consensus panel. MAFLD: Consensus proposed nomenclature for metabolic-associated fatty liver disease. Department of Gastroenterology 2020; 158 : 1999-2014. e1. [ PubMed ] [ DOI ] [ Quoted in this article: 1 ] [ Quoted by CrossRef: 304 ]