This is an automatically translated article.
The article was professionally consulted with Master, Doctor Do Xuan Chien - Head of Department of Medical Examination & Internal Medicine - Vinmec Ha Long International General Hospital.The target fasting blood sugar should be between 3.9 and 6.7 mmol/l and the concentration 2 hours after a meal should be < 7.8 mmol/l. For the elderly, the glycemic target is 5.6 to 8.3 mmol/l fasting and < 11.1 mmol/l after meals. For pregnant women, the glycemic target is < 5.3 mmol/l before meals and < 6.7 mmol/l after meals.
1. Use insulin safely
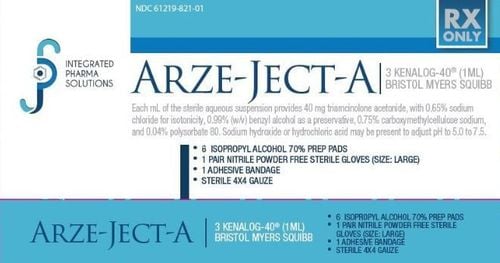
1.1. Using insulin Regular insulin (regular insulin) is not concentrated is the only type of insulin that can be used for intravenous infusion in emergency situations. Do not use other types of insulin for intravenous administration because it can cause a life-threatening hypersensitivity reaction.
When it is necessary to mix 2 types of insulin, the regular insulin should be drawn into the syringe first.
When administered intravenously, only regular insulin should be mixed with isotonic saline to achieve a concentration of 1 unit of insulin/ml. Inject slowly intravenously every 50 units for a minimum of 1 minute.
It is necessary to rotate the injection sites under the skin to avoid lipodystrophy.
Mixtures of regular insulin and NPH insulin, or regular insulin and slow insulin, should be injected within 5 to 15 minutes of mixing.
1.2 Injection technique Insulin vials and insulin syringes : If the insulin product is in suspension (turbidity like milk), it should be shaken gently about 10 times to return the drug to the suspension form after settling. With rapid-acting insulin, shaking may not be necessary since the preparation is already in the form of a clear solution. Disinfect the insulin vial cap with a cotton ball dipped in the disinfectant solution. Before withdrawing insulin, draw air into the syringe with a volume equal to the required dose of insulin. Pump the sucked air into the insulin vial. Take the insulin gently, avoiding swirling the solution in the vial. Remove air bubbles.
Insulin pen: With insulin suspension, it is necessary to gently shake the pen about 10 times to evenly distribute the slow-acting insulin suspension. Insert the injection into the injection pen. Turn the injection pen to 2 units. First of all, these 2 units must be pumped to remove air bubbles in the syringe until you see a drop of water at the tip of the injection pen. If not, do it again, until you see a drop of water at the tip of the injection. Select the corresponding insulin dose level and inject.
1.3 Choose injection site The fastest absorption site is the abdomen, followed by the arm. However buttock is also an injectable site, but so far there have been no studies on the time of absorption in the buttock area. This difference in absorption time is used to prolong or shorten the duration of insulin action.
Pay attention to use alcohol-soaked cotton swabs to disinfect the skin before injecting.
Varies around injection sites (can keep the same injection site at a given injection hour) or rotates on the same injection site, injecting at sites about 2 to 3 cm apart.
The duration of action of rapid insulin can be shortened by injecting it in the abdomen or prolonging its duration by injecting it into the thigh. Injected into the arm for a medium duration of action
Inject at an angle of 90° or 45°, can be injected at normal state or gently pull the skin at the injection site.
Wait 10 seconds before withdrawing the injection so that the insulin can diffuse.
The needle should be withdrawn quickly to avoid causing insulin to escape at the injection site.
Target fasting blood sugar between 3.9 and 6.7 mmol/l and concentration 2 hours after a meal should be < 7.8 mmol/l. For the elderly, the glycemic target is 5.6 to 8.3 mmol/l fasting and < 11.1 mmol/l after meals. For pregnant women, the glycemic target is < 5.3 mmol/l before meals and < 6.7 mmol/l after meals. Monitor HbA1c every 3 months. This index reflects the average value of blood glucose levels over 3 months. The goal is < 6.5% to 7% in cases where diabetes is well controlled.
1.4 Adjust insulin dose Review your treatment by adjusting insulin dose based on blood glucose results after insulin treatment in the previous days.
Anticipate situations affecting blood sugar: adjust dose based on anticipating unusual physical activity or next meal.

2. Some other notes when using insulin for people with diabetes
Diabetics who have to inject insulin often wonder how to use the drug most effectively. Therefore, knowing how to use insulin in a scientific and correct way, helping to absorb the drug well is very important in the treatment of diabetes.
Intramuscular injection helps insulin to be absorbed and work faster. However, intramuscular injection is not a common route of administration and it has its own risks. Do not inject intramuscularly into areas with a thick layer of fat, for intramuscular injections, a longer needle should be used to allow the needle to reach the muscle. Thin people can use a regular subcutaneous needle for intramuscular injection.
Exercise that moves the muscles of the insulin injection site will increase insulin absorption. For example, if you run after injecting insulin in your thighs, you will absorb insulin faster. Massaging the injection site has a similar effect.

Ketoacidosis tends to increase insulin absorption resulting in a more rapidly acting insulin which is beneficial for patients as they need to lower their blood sugar as quickly as possible.
The rate at which insulin is absorbed is not the same between people. For example, when injecting semi-slow insulin (lente, NPH), the drug works for 16-20 hours, but in some people it is only 8-10 hours. Compared between different days, even with the same person receiving the same insulin, the same insulin dose at the same site, the duration of action can be changed by up to 50%, while the time to peak effect can be changed by 25 - 50%.
With small doses of 5 - 10 units, there is no difference but with higher doses, eg 20 units, insulin will be absorbed more slowly than 10 units. However, the difference was most pronounced when injecting high doses of 100 units of insulin or more. Similarly, injections of high-concentration insulins (U 100 or U 500) will cause the drug to be absorbed more slowly than with lower-strength insulins (U 40).
It is best to inject insulin before meals. Depending on the type of insulin, the time from injection to eating is different. For example, with regular insulin (regular) is 20-30 minutes, insulin mixtard is also 30 minutes, semi-slow insulin (lente, NPH, insulatard...) is 60 minutes. If the patient eats later, the patient is at a very high risk of hypoglycemia.
There will be some insulin ineffective because part of the injected insulin is broken down (destroyed) by enzymes present in the subcutaneous tissue. In most patients this amount of insulin is very small and does not affect the overall effect and does not require an increase in dose. However, in a very small number of patients, the breakdown of insulin in the subcutaneous tissue is very large, so to achieve the goal of glycemic control they must inject insulin in very large doses, possibly up to 200 units. . This does not occur if insulin is injected intravenously. It can be overcome by injecting insulin with an enzyme inhibitor called trasylol but this drug is very expensive, so the simplest and most effective way is to inject more insulin.
Roll the vial (or injection pen) that warms and mixes the insulin. Only rolling the vial of semi-slow insulin (lente, NPH or latard) or insulin mixtard is recommended, with regular (regular) insulin not required. The insulin vial should not be shaken vigorously because air bubbles can easily be created and when the insulin is drawn into the syringe, air may enter the syringe.
Some patients with diabetes are able to self-adjust insulin injections (increase or decrease) according to food intake. Note that people who do not have good knowledge or are not guided by a specialist should not apply this method to avoid the risk of hypoglycemia.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.