This is an automatically translated article.
Posted by Doctor Mai Vien Phuong - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General HospitalThe vague presentation of microscopic colitis is similar to celiac disease, irritable bowel syndrome (IBS), or inflammatory bowel disease (inflammatory bowel disease). Its diagnosis can be further complicated if celiac disease or concomitant inflammatory bowel disease is present. Treatment is usually aimed at shortening the duration of symptoms. In this article, we will discuss diagnostic methods, problems that make diagnosis and current treatment difficult.
1. Definition
Microscopic colitis is a chronic inflammatory bowel disease characterized by clinical presentation of chronic diarrhea, but the patient has a normal colonoscopy and the diagnosis can only be made on histological basis. learn. Microscopic colitis is divided into two groups of collagenous colitis and lymphocytic colitis.2. Classification
The term microscopic colitis covers two separate diagnoses: lymphocytic colitis and collagenous colitis. The name describes a change in the colonic mucosa that is not due to an infectious cause that ultimately causes chronic, non-bloody diarrhea in the absence of other physical findings. It affects women more commonly than men and manifests usually over the age of 65. Microscopic colitis can be confused with diseases with similar manifestations, such as celiac disease, IBS, or inflammatory bowel disease.
3. The role of pathology in disease diagnosis
Colonoscopy is usually normal and a biopsy of the colonic mucosa is required for a definitive diagnosis. Collagenous colitis can be easily distinguished from lymphoid colitis by the presence of a thick subepithelial band of collagen while the hallmark of lymphoid colitis is an infiltration of the colonic epithelium with epithelial cells. lymphocytes.
These two conditions of microscopic colitis are associated with other autoimmune disorders such as celiac disease, rheumatoid arthritis, thyroid disease, or diabetes. In patients with concomitant celiac disease or inflammatory bowel disease, the diagnosis of microscopic colitis is often difficult. The goal of treatment is to shorten the duration and control symptoms and can be done successfully in most cases. In this article, we will discuss current diagnostic methods, confounding problems, and treatment.

4. Clinical definition
Microscopic colitis is defined by symptoms of chronic diarrhea, watery diarrhea without an identifiable cause of infection, often without endoscopic lesions or radiographic findings but only abnormalities of the colon. histology.
5. Epidemiology
With increased awareness and improved diagnostic capabilities, microscopic colitis has become a common diagnosis. The incidence of microscopic colitis is 10/100,000 in the United States. Lymphatic colitis is slightly more common and has an incidence of 5.5/100,000, while membranous colitis currently has an incidence of 4.6/100,000. The median age at diagnosis of microscopic colitis is that patients aged 60-65 and over 65 years have a 5-fold increased risk of developing microscopic colitis. Other risk factors for developing microscopic colitis include female sex, a history of malignancy, hypothyroidism, or celiac disease.
6. Pathogenesis
The etiology is multifactorial and the exact mechanism is unknown. However, it is believed that the unregulated immune response to the luminescent agent results in decreased sodium and chloride absorption as well as active chloride excretion. Diarrhea can be defined as discharge.
One study showed that the thick band of collagen found in collagenous colitis can act as a diffusion barrier and regulate tight splicing molecules down. Drugs that have been implicated in causing microscopic colitis include H2 blockers, potent acid secretion inhibitors, SSRIs, carbamazepine, simvastatin, and ticlopidine. Lansoprazole, for example, a potent and commonly used acid-secreting inhibitor, has been extensively studied for its association with microscopic colitis. A case study of 850 patients converted from omeprazole to lansoprazole showed a direct correlation of lansoprazole with intermittent diarrhea characterized as lymphocytic and collagenous colitis histologically. When lansoprazole was discontinued, subsequent biopsies showed resolution with normalization of colon histology.

7. Clinical results
Symptoms may include some or all of the following: intermittent or persistent watery diarrhea, abdominal cramps, urgent or involuntary stools, weight loss or nausea. A complete history helps distinguish this disease from other causes of chronic, watery diarrhea. It's important to get a complete list of medications, including both prescription and over-the-counter drugs. Physical examination is usually unremarkable.
Laboratory findings are generally not useful for diagnosis or assessment of disease activity. The first step should be to collect a stool sample. Although not routinely used for diagnosis, an increased number of CD3+ T cells are found in the stroma and intraepithelial cavity in both lymphocytic colitis and colloidal colitis or GnRH-R, which is seen in IBS is infrequently observed in patients with microscopic colitis. Interestingly, there was an increase in the rate of HLA DQ2 in both subtypes of microscopic colitis.
8. Diagnostic modalities
Test of choice is colonoscopy with biopsy. Histology of colon (colon) biopsy shows mucosal inflammation and thickening of the subepithelial collagen, as in collagenous colitis, or an increase in the number of lymphocytes in the superficial epithelium. as in lymphocytic colitis. Flexible sigmoidoscopy may be sufficient; however, negative results do not exclude the possibility of this disease. It is important to perform multiple biopsies throughout the colon, because histiocytic and lymphoid colitis can be patchy. However, more than 90% of the findings were in the left colon.
9. Endoscopy and pathology
Colonoscopy is usually completely normal. However, a rough and nodular mucosal surface may be seen in IBD. Congestion and vascular torsion with diffuse mucosal laxity have been noted in the early development of collagenous colitis. Mild edema and vascular loss may be seen. The appearance of “linear lacerations” of the colonic mucosa may occur in collagenous colitis, also defined as “mucous lacerations”. This finding was explained by trauma to the colon resulting in decreased elasticity due to the stiffness of collagen subepithelium. Histologically, collagenous colitis is described by collagenous deposits under the colonic mucosal epithelium 7-100 micrometers in diameter (normally 1-7 micrometers). A common finding is that the subepithelial collagen layer is larger than 10 micrometers. Lymphocytic colitis is characterized by a monocyte infiltrate with few neutrophils and eosinophils in the stroma and intraepithelial lymphocytes greater than 20 per 100 surface epithelial cells (normally 3-5/100 cells). Occasionally, focal pleurisy is present. Epithelial damage, such as cell shedding and mucin depletion, may occur.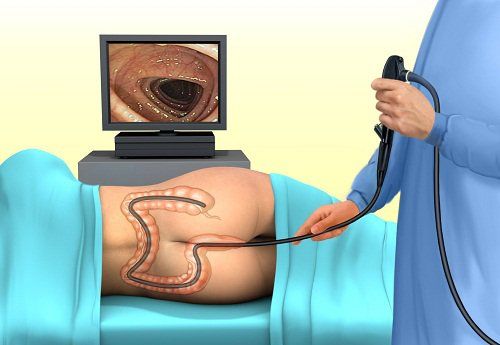
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, owning many machines in the world, helps to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors effectively. best. The hospital space is designed according to hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
References
Lina Vigren, Martin Olesen, et al. An epidemiological study of collagenous colitis in southern Sweden from 2001-2010. World J Gastroenterol. 2012 June 14; 18(22): 2821–2826. Gianluca Ianiro, Giovanni Cammarota, Luca Valerio, Brigida Eleonora Annicchiarico, Alessandro Milani, Massimo Siciliano and Antonio Gasbarrini. Microscopic colitis . World J Gastroenterol. 2012 November 21; 18(43): 6206-6215. Jegadeesan. Microscopic colitis. Is it a spectrum of inflammatory bowel disease. World J Gastroenterol. 2013 July 14; 19(26) Monina F. Pascua, Prashant Kedia, Mark G. Weiner, John Holmes, Jonas Ellenberg, and James D. Lewis, Microscopic colitis and Medication Use .Clin Med Insights Gastroenterol. 2010 May 18; 2010(3): 11–19. Pardi DS, Loftus EV Jr, Smyrk TC, et al. The epidemiology of microscopic colitis: a population based study in Olmsted County, Minnesota. Gut. 2007;56(4):504 Marina Kim, Archana Patel, Diagnosis and Management of Microscopic Colitis: A Review of the Literature, Inflammatory bowel disease: a practical approach, Series
87, Practical Gastroenterology • february 2014