This is an automatically translated article.
Posted by Dr. Tran Hoang Ngoc Anh - General Surgery Department - Vinmec Central Park International General Hospital
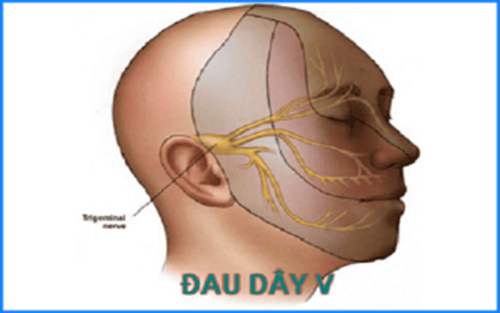
In recent years, with the development of medicine and especially the treatment regimen for nerve pain V resistant to medical treatment has been used in the past 15 years, including interventional techniques such as: The methods of percutaneous intervention (Gasser ganglion thermocoagulation, glycerol injection into the cerebrospinal fluid pool, balloon insertion of Gasser ganglion), some authors use a direct approach such as (microsurgical partial resection of the branches). major nerves, microvascular decompression surgery)
The first person to effectively treat primary V neuralgia was a neurologist BERGOUIGNANT, who recommended the use of antiepileptic drugs (Phenyl-hydantoine). In 1962, BLOM announced the spectacularly effective treatment with Carbamazepine (Tegretol), which is still the drug of choice for the medical treatment of V neuralgia. More recently, FROM et al., 1980, there was evidence that the efficacy of Baclofen (Lioresal) further increased the activity of Tegretol. Other treatments are only supportive and they are used only in cases of intolerance to Carbamazepine or to Baclofen. Only when neuropathic pain becomes resistant to medical therapy, or only when medical therapy is not well tolerated, is surgical intervention such as percutaneous or next-line interventions indicated. direct access.
1. Medical treatment
Like the majority of pain of nerve origin, neuropathic pain V will not respond to conventional analgesia and is resistant to morphine. However, some psychotropic and psychotropic drugs are effective when taken.
The drug of first choice in this condition is carbamazepine (Tegretol). The dose is adjusted to ensure effective treatment with the fewest side effects and the dose used varies from patient to patient. Usually the dose is adjusted to range from 0.6-1.8 g/day.
Some other drugs are also effective but only used in cases of intolerance or side effects related to carbamazepine use (allergies, agranulocytosis...). these include drugs such as baclofene (lioresal), some anti-seizure medications such as phenytoine (Di-Hydan), clonazepam (Rivotril), or gabapentine (Neurontine), certain antipsychotic drugs such as levopromazine (Norinan), or Haloperidol ( Haldol), certain anti-anxiety medications or antidepressants such as clomipramine (Anafranil), or amitryptiline (Laroxyl).
2. Percutaneous interventions
2.1 Percutaneous Vth Nerve Thermocoagulation
The most commonly used percutaneous method is percutaneous V nerve coagulation. In the review of SWEET in 1969, the author suggested this method based on 2 theoretical foundations:
First, there is the distribution of autonomic nerve V in the Gasser ganglia and the postganglionic part to the roots. So it is possible that, if we correctly place the uncoated part of the electrode, we get an anatomically selective effect over the painful area. The second is corresponding when creating a thermal lesion (between 60 and 80 °C) on a sensory nerve fiber, which alters the conduction continuity of small-diameter fibers A delta and C compared with fibers with large aperture myelinated A beta and gamma. This destruction is usually predominant in somatic sensory fibers, as has been demonstrated in animals as well as in human electrophysiological studies. Technique:
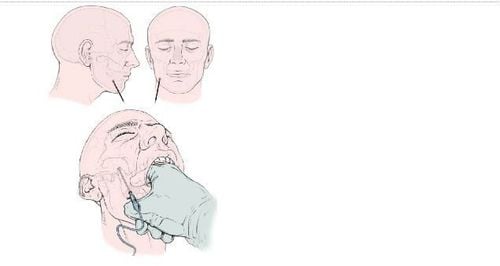
After inserting the percutaneous needle through the cheek to the foramen ovale under C-Arm control, perform thermocoagulation in the post-Gasser ganglion medial part of nerve V. Autopsychological distribution of the The branch of nerve V in this position allows electrode placement and only thermocoagulation on the corresponding nerve fibers according to the distribution of pain. The precise positioning of the electrode is controlled under the C-arm and electrical nerve stimulation. When electrical stimulation of the nerve causes numbness in the sensory distribution corresponding to the stimulated fibers. It is only when needle puncture through the foramen ovale and thermodynamic period is necessary that general anesthesia by short-acting intravenous route (1-2 minutes each time), without intubation.
When passing the foramen ovale, the electrode is pushed up posteriorly and inward until the tip of the needle is slightly past the superior crest of the stony bone and slightly to the back of the slope. According to the anatomical distribution, this position corresponds to the junction between the triangular plexus and the posterior root, which is the exit of the V nerve from the Meckel's fossa in the cerebellar pontine angle. According to the experience of some authors, when the cerebrospinal fluid is seen flowing out of the trocar, the electrode position is right in the trigeminal cerebrospinal fluid pool. Neurophysiological localization performed by electrical and thermal stimulation was in all cases an important factor. Electrical stimulation induces paresthesia in the distribution of sensory fibers corresponding to the pain region, allowing confirmation of the location of the electrode immediately or adjacent to the nerve fibers to be coagulated. We consider this test valid only if the threshold of the electrode producing paresthesia must be below or equal to 0.2 volts. If an electrode threshold is significantly high, it is evidence that the electrode position is quite far away.
Research results of a few authors have a large number of patients in the literature such as French authors (PERTUISET, 1977; THUREL, 1977; SIEGFRIED 1981) and in other countries' literature (SWEET, 1974; ONOFRIO, 1975; TEW 1982) had no mortality. The majority of patients were cured of their neuropathic pain (immediate success 88%-100%, recurrence 13%-29%, depending on study).
Relatively low complication rate (severe sensory disturbances: 0.5-3%, conjunctivitis: 0-5%, ophthalmomotor paralysis: 0-1%), and acceptable secondary effects can be (mild sensory disturbances: from 3 to 26%, decreased corneal sensation without causing conjunctivitis: 1-10%, transient occipital muscle paralysis 2-3%, transient ophthalmoplegia 0-3%.
2.2 Microvascular decompression
First performed by Gardner 1959, after Dandy 1934 and later Lazorthes emphasized the search for vascular and neurological conflicts in patients with neuralgia primary V in the cerebellar pontine angle, however, microvascular decompression of the V nerve was systematized and popularized by Jeanette in the 1970s. Since then, there has always been controversy between the role of impulses neurosurgery as well as the effectiveness of microvascular decompression surgery.
In the study of Decq et al. over 400 cases, analysis of the first 150 cases with direct access to the cerebellar pontine angle was performed on patients with facial nerve pain and followed for more than 3 years. There was a neurovascular conflict present in 132 cases, nerve compression due to other lesions was seen in 14 cases, accounting for 97% of cases. This rate of 97% also shows more significance when surveying a group of 52 patients who underwent parapontine nerve root partial resection to treat facial pain due to tumor proliferation, we did not find a conflict. However, in an anatomical study by the authors HARDY and ROHTON as well as MERCIER, it was found that there was a vascular loop that inserted into the V nerve, but in fact, this patient did not have any abnormalities when he was alive. presence of neuropathic pain V.
Technique:
Surgery is performed under general anaesthesia, performing a small craniotomy into the cerebellar pontine angle to allow access to the V nerve and release the nerve This sutra with one or more incompatible elements, maintain a distance between the structures by placing between them a small piece of Dacron or preferably a piece of Teflon. Regardless of the technique, the goal is always the same: Move from anatomical incompatibility back to normal if possible. During arterial dissection, under no circumstances should the perforating branches reach the brain stem and manipulate the vascular loop gently to avoid causing this vasospasm.

Of the 150 cases in the initial analysis, there were actually 14 cases of symptomatic neuropathic pain, which were cured of neuropathic pain by complete resection of the lesion in 11 patients and by root resection, respectively. or V nerve thermocoagulation in 3 other cases. Of the 136 cases of primary neuropathic pain, only 4 had no anatomical abnormalities detected in the cerebellar pontine angle. In these four cases, neuropathic pain was successfully treated by hemiparesis of the parapontine roots. In 132 cases with vascular compression factor, 17 cases required partial root resection, because the nerve was not decompressed as well as transferring the corresponding vascular components. In which, there were 9 cases of dilated basal vertebral artery that could not be separated and the remaining 8 cases of a cerebellar artery that was difficult to separate to maintain a distance from nerve V. Thus, the total number of patients was Perform microvascular decompression surgery is 115 cases analyzed results. In these 115 cases, 65% of the patients presented with pure paroxysmal pain, the remaining 35% presented a state of persistent umbilical pain of the burning pattern associated with neuropathic pain. Follow-up for a period of 1-6 years, microvascular decompression surgery completely cured pain symptoms in 83.2% of cases and 3.5% of cases, surgery could suppress paroxysmal pain but still leaves a persistent navel pain state. In addition, 2.7% of surgical cases had a slight improvement, requiring the use of more drugs, but the dose was reduced. In the study group, there were 4.4% failure right after surgery and 3.5% recurrence cases. Comparing the results of Decq et al with other authors showed that the effectiveness of microvascular decompression surgery in the treatment of neuropathic pain is relatively similar. Relatively similar mortality, within 1%, is usually cerebellar infarction.
3. Summary
Which intervention method to choose: The direct approach or the percutaneous approach to the treatment of neuropathic pain V that is resistant to medical treatment so far has not had a satisfactory answer. There is really no such thing as the best method, but when there are many treatment techniques in hand, for each patient we will choose a method that gives the patient the best effect.
In clinical practice we encounter three situations:
When the patient is elderly or in poor condition, in this case it is suitable to perform a percutaneous method, but the patient must have sensory impairment on the initial pain distribution. The most reliable percutaneous method is still thermocoagulation, but nerve interpretation of the Gasser ganglion by Glyceron or balloon compression is also preferred by some authors. Percutaneous therapy is also the treatment of choice in patients who have plaque sclerosis and present a medically refractory paroxysmal facial pain. On the contrary, when seeing a young patient, especially when the patient presents with facial nerve pain distributed along the V1 arm, the doctor may perform microvascular decompression surgery to resolve the pain and not yield a secondary sensory defect and avoid a nonspecific destructive approach. Given the fact that a large proportion of patients present with an intermediate setting, it is difficult to decide whether a percutaneous approach or a direct intervention approach. In this situation, the choice of treatment method is based on the surgeon's experience as well as the patient's choice to choose the appropriate treatment method. Vinmec International General Hospital with a system of modern facilities, medical equipment and a team of experts and doctors with many years of experience in medical examination and treatment, patients can rest assured to visit. and treatment of migraine, neuralgia at the Hospital.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORE
Why do you have 5th nerve pain? Features of nerve pain V No. 8 Nerve tumor 8: causes and treatment