This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalIncontinence is defined as the involuntary passage of rectal substances (solid or liquid stools) through the anal canal and the inability to delay evacuation until it is socially convenient.
Fecal incontinence is considered a common disorder with a significant economic burden, but because of the confusion it is often underreported. Fecal incontinence seriously affects the patient's quality of life, leading to organic and psychological comorbidities. A detailed history and examination by the physician are required to identify the patient's primary complaints with a focus on risk factors for fecal incontinence and whether passive or impulsive fecal incontinence predominates. so or not. Furthermore, finger rectal examination is paramount to assess anorectal sensation, anal sphincter rest, and importantly, squeeze pressure.
To diagnose fecal incontinence, doctors often use the following methods:
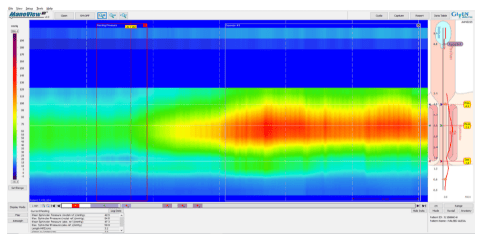
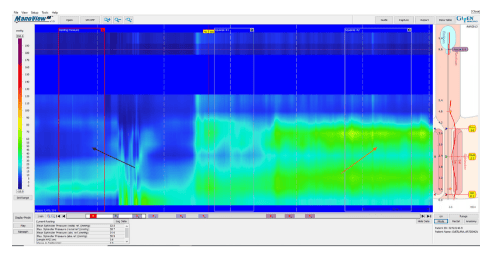
1. High-resolution anorectal manometry HRAM
According to American College of Gastroenterology guidelines, in cases of fecal incontinence, testing with high-resolution anorectal manometry is recommended. High-resolution anorectal manometry is an important diagnostic tool for assessing anorectal motor function and sensation. The use of high-resolution anorectal manometry is an essential diagnostic tool in the evaluation of fecal incontinence, as it improves understanding of the underlying pathophysiological bases of fecal incontinence, for to provide optimal therapy for each specific patient. High-resolution anorectal manometry, which provides dynamic recording of the anal sphincter and anorectal pressure, is considered the best established diagnostic tool allowing for objective assessment several elements of anal and rectal function including basal tone and contractility, anal-anal coordination, and reflex function (such as inhibitory anal regurgitation) as well as rectal sensory threshold, is an important predictor of response to biofeedback training.
2. London consensus on anorectal manometry procedure and analysis
The recently established International Organization for Anal Physiology Research has published a consensus guideline recommending a de facto standardized procedure for performing and analyzing anorectal manometers, named the London Classification. Some of the manometry findings that may be related to fecal incontinence include decreased anal sphincter resting pressure (hypotension) and inotropic impairment (decreased contractility). Furthermore, high-resolution anorectal manometry allows the assessment of abnormal rectal sensitivity for both hypersensitivity and hypersensitivity, two conditions that can cause fecal incontinence in different manners. Rectal sensation is assessed by inflating a balloon in the rectum and recording the balloon volume required to produce the first sensation, urge, and discomfort. Rectal allergies can be caused by neuropathy, mucositis, or fibrosis and can make the patient unaware of the presence of stool in the rectum, leading to stool accumulation and fecal incontinence. Rectal hypersensitivity can lead to urinary incontinence and is common in patients with irritable bowel syndrome
3. Imaging of the pelvic floor and anal canal
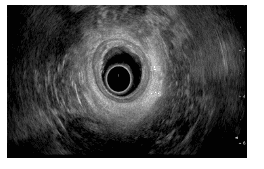
In patients with uncontrolled anal pressure drop, especially when considering surgery, the anatomical integrity of the anal sphincter, rectal wall, and anal muscle region should be evaluated by ultrasonography. endoscopy or MRI. Although, both tests are considered to be overlap in identifying abnormalities including scarring, defects, thinning, or marked focal atrophy, nevertheless, every test is unique and diagnostic. . While ultrasound is superior in identifying an internal anal sphincter tear, external anal sphincter atrophy is more identified by MRI. In addition, it is better to distinguish between tears and scarring of the external anal sphincter with MRI.
Anal duct ultrasonography:
TRUS or anal ultrasound (EAUS) is a simple, well tolerated, widely available test that is considered the gold standard in examining the integrity of the anal sphincter. subject. However, its sensitivity and accuracy in determining sphincter injury are controversial and operator dependent. Gold et al. reported that host-to-server agreement in the diagnosis of sphincter defect and measurement of the intraanal sphincter by anal ultrasound was very good, and better than that of the anal sphincter measurement.
Common structural problems in patients with fecal incontinence that are readily identified by anal ultrasound include disruption of the anal sphincter (defect), and atrophy of the internal anal sphincter (as determined by the presence of a defect). Diffuse thinning of the sphincter to a thickness of less than 1 mm, and discontinuity (defective) or scarring presenting as focal thinning. Difficulty with anal ultrasound due to the inability to define the outer anal sphincter boundary and the inability to distinguish between normal muscle tissue and fatty infiltration. by a diffuse reduction in muscle mass on serial images below the anorectal level, to the point where muscle is virtually unidentifiable.The leading cause of fecal incontinence is anal sphincteric injury resulting from vaginal delivery in women, and it can be caused by direct tearing of the anal sphincter or indirectly by damage to the internal sphincter
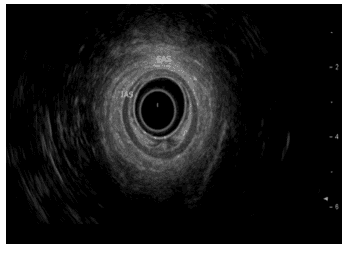
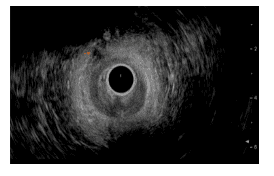
Source: Department of Gastroenterology, Galilee Medical Center, Nahariya, Israel. EAS : External anal sphincter; IAS: Intra anal sphincter.
Two-dimensional anal canal ultrasound:
This technique allows cross-sectional images only in the axial plane, which remains the mainstay of sphincter examination; however it does not achieve the precise longitudinal measurements required for complete surgical intervention planning. On the other hand, a three-dimensional anal canal ultrasound allows length, thickness, area and volume measurements to be determined by creating a fingertip mass that can be seen from any plane and is displayed as multifocal or tomographic images, thus allowing more accurate defect visualization.
MRI: MRI is expensive, not readily available, and is not accepted by anaerobic patients and is not appropriate in patients with pacemakers, defibrillators, and other metal implants. Two modalities of MRI are available in clinical practice: invasive endothelial MRI using endothelial coil and noninvasive external phase array. Both modalities are comparable in identifying external anal sphincter defects and atrophy. Compared with anal ultrasound, the accuracy of intra-anal sphincter MRI is lower in the diagnosis of anal sphincter defects. Several studies have reported that anal canal ultrasound and endometrial MRI are equivalent in the diagnosis of external anal sphincter injury; however, endorectal MRI allows better differentiation between fat and muscle and identifies scarring. This feature highlights the diagnostic power of anal ultrasound in detecting structural damage and focal thinning of the external anal sphincter. Interestingly, only moderate agreement between anal ultrasound and external array MRI in the diagnosis of obstetric trauma, which represents the main cause of fecal incontinence, has been reported. Recently, magnetic resonance defecation has gradually emerged as a modern alternative to traditional X-ray-based defecation.
3. Capture the process of defecation by magnetic resonance
This is a non-invasive test that uses MRI to obtain images at different stages of the bowel movement to assess the functioning of the pelvic muscles and provide insights into the function of the bowel. rectal function. Magnetic resonance fecalography can provide important functional disorders related to defecation as well as various important structural abnormalities associated with fecal incontinence and other pelvic floor disorders. These structural abnormalities include anorectal, intestinal epithelium, anorectal prolapse, and perineum descending. The determination can affect the type of surgical treatment.
4. Electrophysiological neurophysiology of the anorectal
Electromyographic evaluation of the neurophysiology of the anorectal tract includes evaluation of dorsal and spinal nerve conduction using the EMG sphincter examination. This test is of particular significance when surgery is being considered; however its availability is mainly for research purposes and its clinical application has recently decreased in many countries. However, the use of EMG has been advocated in patients with bothersome symptoms suspected of stemming from neurosphincteric weakness, particularly when it is thought to be due to sacral root injury. We support the assessment of rectal sensation and EMG needle compliance of the anal sphincter.
Conclusion
High-resolution anorectal manometry is an important initial diagnostic modality to begin with, as it can provide important information about the functions of the anal sphincter and sphincter. Rectal palpation can be assessed using an intrarectal dilatation balloon. The anatomical integrity of the anal sphincter, rectal wall, and anorectal muscle area should be evaluated by anal ultrasound or MRI.
Although, both tests are considered to be overlapping in identifying abnormalities including scarring, defects, atrophy, or markedly localized thinning, each test has its own uniqueness and diagnostic capacity . While anal canal ultrasound is superior in identifying an internal sphincter tear, external anal sphincter atrophy is better defined by MRI. In addition, it is better to distinguish between tears and scarring of the external anal sphincter with MRI. The role of EMG in the evaluation of fecal incontinence needs to be explored. Ultimately, this recommended approach will assist clinicians in the step-by-step management of patients with fecal incontinence.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.














