This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Urinary incontinence (fecal incontinence) is a common debilitating end result of a number of diseases that affect quality of life and lead to disability, disease and increased burden on society. Because of the different causes of fecal incontinence, it is important to evaluate and identify the underlying pathogenesis.
Some of the investigative tools available include high-resolution anorectal manometry, transrectal ultrasound, magnetic resonance imaging, and electromyography. This review provides an overview of the etiology and pathophysiology of fecal incontinence and expert perspectives on the step-by-step investigation of patients with fecal incontinence based on the available literature. In general, a high-resolution anorectal manometer should be the first investigational tool for fecal incontinence, followed by transrectal ultrasonography or magnetic resonance imaging to look for intraanal sphincter lesions and lesions. injury to the external anal sphincter.
1. What is fecal incontinence?
Incontinence is defined as the involuntary passage of rectal substances (solid or liquid stools) through the anal canal and the inability to delay evacuation until it is socially convenient. Important factors to consider when determining fecal incontinence include duration of symptoms of at least 1 month and age of onset of at least 4 years with previously achieved control. fecal incontinence is considered a common disorder with a significant economic burden, but because of embarrassment, it is often underreported; Therefore, its true popularity is a challenge to assess.
Són phân là gì?
Frequency
The prevalence of fecal incontinence in the US adult population is estimated to be 0.8%-6.2%. The incidence of fecal incontinence increased with age from about 3% in the 20-29 year old group to 16% in those ≥ 70 years old. A systematic review by Sharma et al of 30 studies estimated the prevalence to be 1.4% to 19.5%. This difference was clarified by the variance in the data collection methods applied and the definition of fecal incontinence. Not surprisingly, the incidence of fecal incontinence reported in individual interviews was lower than in anonymous questionnaires. The incidence of fecal incontinence is similar in both men and women, while the pathogenesis is often not the same between sexes.
2. Impact of fecal incontinence on life
Diarrhea has important consequences for social functioning and quality of life as well as a significant economic burden due to diagnosis, medications, equipment, procedures and reduced working capacity. Fecal incontinence is often classified from a clinical point of view as: fecal incontinence (discharge despite active efforts to contract the anal sphincter), passive incontinence (incontinence without discharge). recognizable), and fecal leakage (leakage of stool with normal contraction and movement).
Many comorbidities and conditions are associated with fecal incontinence such as anal sphincter dysfunction, rectal disorders, neurological disease, malignancy, mental illness, and others. A major challenge in the management of fecal incontinence is the confusion between the objective and subjective parameters.
3. Causes and risk factors of fecal incontinence

Người mắc bệnh ruột kích thích có nguy cơ bị són phân
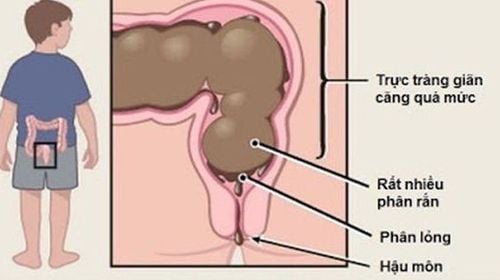
Fecal incontinence represents a final pathway of a number of traumatic and non-traumatic disorders. The most non-traumatic causes include anal sphincteric disease and rectal dysfunction as well as inflammatory, congenital, structural, metabolic, neurological, muscular, psychological, and functional diseases. difference. Changes in bowel habits, such as diarrhea for any reason (including inflammatory bowel disease, irritable bowel disease) and constipation accompanied by paradoxical diarrhea and fecal incontinence are considered to be among the most common risk factors for fecal incontinence.
The most common causes of structural trauma to the anal sphincter leading to fecal incontinence are related to obstetric trauma during vaginal delivery, anorectal surgical procedures including anorectal dilatation, Hemorrhoidectomy, fistula resection, fistula resection, sphincterotomy, rectal prolapse and ileal reconstruction surgery. Many patients with neurological disorders affecting the brain, spinal cord, or peripheral nervous system experience fecal incontinence because of impaired control of the anal sphincter, reduced or absent anorectal sensation, or abnormal reflexes. in the rectum. Diabetics may have neuropathy of the anal canal and some have chronic diarrhea. Connective tissue diseases, notable scleroderma, myopathy, and atrophy of the internal anal sphincter (the internal anal sphincter) can lead to fecal incontinence. Rectal surgery can disrupt the function of the rectum as seen in patients after anterior resection. In addition, pelvic radiation therapy can lead to fecal incontinence.
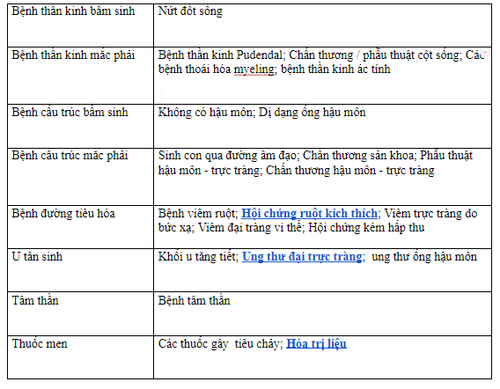
4. Organic causes of fecal incontinence.
5. History check and clinical examination
It is important in the early stages of the evaluation of fecal incontinence to look for possible causes and risk factors during a careful detailed history review to route the diagnosis accordingly. The main symptom of fecal incontinence is a progressive loss of control over substances in the rectum including solid and liquid stools. Urgency is defined by the patient's awareness of the urge to defecate but the inability to contract sufficiently the external anal sphincter (the external anal sphincter) until defecation, and many diseases People report “accidents” within seconds or minutes. Unrecognized involuntary discharge is classified as passive consumption and is often due to disturbed sensation of the rectum and anal canal. It is imperative to identify discrete disparities related to different triggers, such as day versus night, physical activity, cough, stress, stool consistency, or food intake.
Additional symptoms
Other side effects of fecal incontinence that can arise from fecal leakage include itching, irritation of the skin around the anus, and infection as well as urinary tract infections. Notably, these secondary symptoms may be the main complaints that prompt patients to seek medical attention without mentioning fecal incontinence. Furthermore, fecal incontinence can have other important associated conditions that necessitate direct patient exploration such as urinary incontinence, vaginal distention (rectum, cyst), rectal prolapse, Change in bowel habits, bowel disorders, and rectal bleeding. Physical examination of the anorectal area is paramount and begins with a visual examination for fecal leakage, skin irritation and infection, hemorrhoids, fistulas, and anal fissures. During rectal examination with a finger, the experienced index finger can make a general estimate of the anal contractile and resting pressures. Furthermore, coordinated relaxation of the pelvic floor muscles during exertion can also be addressed during Valsalva maneuvers to look for possible defecation disorders (i.e. dysphagia). power).