This is an automatically translated article.
The article is professionally consulted by Master, Doctor Nguyen Huy Nhat - Department of Medical Examination & Internal Medicine - Vinmec Danang International General Hospital.
Nosocomial pneumonia is the most common healthcare-associated infection in the ICU and the leading cause of death among nosocomial infections. So what are the measures to prevent hospital-acquired pneumonia? Let's find out through the following article.
1. General information about hospital-acquired pneumonia
Pneumonia caused by drug-resistant bacteria is increasing rapidly, causing difficulties in initial antibiotic treatment, increasing mortality, prolonging hospital stay and increasing treatment costs.Nosocomial pneumonia (VPBV) is pneumonia occurring 48 hours after admission with no previous lesions or progression on chest X-ray before 48 hours of admission.
In Vietnam, the results of a national survey in 2005 on 19 hospitals showed that hospital-acquired pneumonia accounted for the highest rate among other hospital-acquired infections: 55.4% of all hospital-acquired infections.

2. Guidelines for the prevention of hospital-acquired pneumonia
Studies have demonstrated that the implementation of integrated nosocomial pneumonia prevention measures such as improved nosocomial pneumonia prevention measures in the ICU daily; propaganda with pictures, articles to respond to medical staff; reminding everyone to do the same every day has brought a lot of success. Some hospitals have reduced the incidence of nosocomial pneumonia to 1/1000 days of mechanical ventilation through interventions.Implement measures such as reducing aspiration of patients, preventing cross-contamination from healthcare workers' hands, properly disinfecting and sterilizing respiratory tools, educating medical staff and Patients should be taken seriously and fully at domestic hospitals to prevent hospital-acquired pneumonia.
2.1 Training and training Medical staff, as well as students and trainees, must be trained and updated on measures to prevent and control hospital-acquired pneumonia. Patients and visitors should be instructed on measures to prevent hospital-acquired pneumonia.
2.2 Monitoring Monitor periodically or during an outbreak of nosocomial pneumonia in patients at high risk for this disease in intensive care and intensive care units to identify factors such as pathogenic bacteria and antibiotic sensitivity; publish data on infection rates in ICU patients or patients on mechanical ventilation.
The rate of hospital-acquired pneumonia should be calculated according to the number of patients with hospital-acquired pneumonia in 100 days of intensive care or 1 day of mechanical ventilation. Feedback results to hospital leadership, infection control committees, and departments where surveillance is being performed.
Monitor medical staff's compliance with hospital-acquired pneumonia prevention guidelines based on a built-in checklist.
Only perform routine monitoring of culture of specimens, tools and equipment used for respiratory treatment, assessment of lung function, anesthesia when there is an epidemic.
2.3 Disinfection, sterilization of respiratory support equipment Sterilize or disinfect high-level of all tools and equipment in direct or indirect contact with the mucosa of the lower respiratory tract according to the instructions on decontamination. sterilization and sterilization of instruments have been issued; Replace all oxygen breathing lines, masks, and oxygen lines when used for other patients; Routinely disinfect the outside of the ventilator with a moderate disinfectant solution. Periodic maintenance and sterilization of ventilators according to the manufacturer's instructions; Sterilization or high-level disinfection of oxygen humidifiers; High-level disinfection of breathing balls (ambu) after use. Note when sterilizing and sterilizing tools related to aerosol breathing:
Between aerosol sprays on the same patient, instruments must be disinfected at a high level. When used on other patients, the nebulizer must be replaced with a high level of sterilization or sterilization. Use only sterile solution for aerosol spraying. When pouring liquid into the sprayer, it must also follow the principle of aseptic. If the vial is used many times, the manipulation, filling and storage must follow the manufacturer's instructions; Sterilize or high-level disinfection of mouthpieces, tubing, and adapters according to the manufacturer's instructions when used in other patients. Periodic maintenance of the internal components of the spirometer, pulse oximetry meter. Sterilize and sterilize instruments related to anesthesia machines:
Maintain, clean, sterilize or disinfect the components of the anesthesia machine according to the manufacturer's instructions; Disinfect the anesthesia machine's breathing system including the breathing line, CO2 chamber and absorbent, bellows and tubing, humidifiers, pressure limiting valves and other accessories: respirator, reserve ball, humidifying device after use for the patient. 2.4 Prevention of infection by health workers Hand hygiene:
Follow the 5 times of hand hygiene of the World Health Organization, including: After contact with mucous membranes, respiratory secretions or objects contaminated with respiratory secretions with or without gloves; before and after contact with an intubated or tracheostomy patient; before and after contact with any respirator used on a sick person.

Wear gloves when hand contact with respiratory secretions, or tools contaminated with respiratory secretions. Wear sterile gloves when aspirating sputum through endotracheal or tracheostomy.
Change gloves and clean hands between patients, after contact with respiratory secretions or tools contaminated with respiratory secretions, after draining, pouring water in the ventilator line, water trap.
Other protective measures:
Wear a gown when contaminating the patient's respiratory secretions is anticipated, change gown immediately after exposure and before providing care to another patient. Wear a mask, face covering, protective glasses when anticipating the possibility of blood or secretions splashing on the eyes, nose and mouth.
3. Caring for comatose patients, prevention of aspiration pneumonia
Place the patient in the supine position with the head elevated (semirecumbent) 30 degrees - 45 degrees if there are no contraindications; Clean your teeth with an antiseptic solution, preferably 0.12% Chlohexidine. If using a brush, take care of your teeth twice a day; if only gauze is used, take care of the teeth every 2 - 4 hours; Use a sterile sputum suction tube for each suction or a closed sputum suction system if possible. Ideally, each straw should only be inserted into the airway once. Use sterile water to clean the secretions of the sputum suction tube during suction. Do not pump water in before suction. Change the suction hose to the suction hose every day or when used on another patient. Change the aspirator every 4 hours and when used in another patient unless used for a short time (postoperative patients); Regularly check the feeding tube to see if it is in the correct position, assess bowel movements by listening, check the gastric stasis volume to adjust the volume and rate of feeding to avoid reflux, Stop feeding when the stomach is distended or there is no bowel movement.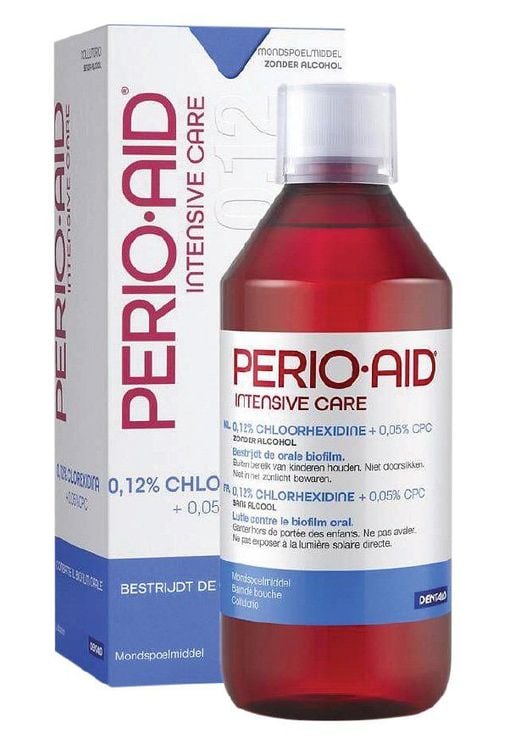
4. Caring for patients with intubation, tracheostomy, other supportive ventilation
Intubated patients Remove secretions from the mouth and pharynx before placing and removing the endotracheal tube. For endotracheal tube with cuff, aspiration must be performed before discharging the cuff; Discontinue tube feeding and extubate the endotracheal tube, remove the tracheostomy tube, nasogastric tube, and jejunal catheter when the indications are exhausted; If prognostication requires long-term intubation, an endotracheal tube with an additional suction wire above the cuff should be used to aspirate secretions from the lower larynx; Pay attention to fix the endotracheal tube well after placement. Tracheostomy patient Tracheostomy under sterile conditions; When replacing a tracheostomy tube: Use aseptic technique and replace with another catheter that has been sterilized or highly disinfected if reused. Change the dressing and fix the tracheostomy with correct technique; Cover the tracheostomy with sterile gauze or a specialized mask. Patients with artificial ventilation Non-invasive ventilatory support should be used for patients if there are no contraindications; Draining and regularly emptying standing water in breathing lines, parts containing standing water, traps water; When aspirating sputum or draining stagnant water in the breathing line, removing the breathing line, care should be taken to avoid backflow of water from the breathing line into the endotracheal tube; The breathing line must be positioned lower than the upper part of the endotracheal tube; Use sterile water to enter the ventilator humidifier. Do not pour water above the specified line level; A heat-humidifier (artificial nose) can be used as an alternative to a heat-humidifier. Routinely replace the heat exchanger every 48 hours. Replace immediately when dirty or dysfunctional; Bacterial filtration should be used between the breathing line and the ventilator to filter bacteria in the inhalation stage and avoid introducing secretions into the ventilator and filter bacteria in the exhalation branch of the breathing line to avoid contaminating the external environment; Replace the breathing tube and the humidifier as soon as it becomes dirty or when it is no longer working properly. Change immediately after use on the patient and disinfect at a high level or sterilize before using on the patient. There is no need for routine replacement of a patient's breathing tube; If a pneumothorax is used, it must be changed daily.5. Respiratory care for patients after surgery
Instruct patients before surgery, especially those at high risk of pneumonia, how to practice coughing and deep breathing; Encourage the postoperative patient to cough frequently, breathe deeply, and change position unless contraindicated. Combining physical therapy for patients at high risk of pneumonia; It is necessary to control postoperative pain well because the pain will make the patient not dare to breathe deeply, cough.6. Other preventive measures

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.