This is an automatically translated article.
The article was professionally consulted with Master, Doctor Dang Xuan Cuong - Department of Emergency Resuscitation - Vinmec Hai Phong International General Hospital.Progressive respiratory distress syndrome is a lung disease, associated with many medical and surgical diseases, can cause multi-organ failure, leading to death if not detected and treated early.
1. What is progressive acute respiratory distress syndrome?
Acute Respiratory Distress Syndrome (ARDS) is a pathological syndrome that describes acute damage to the alveolar capillary membranes of the lungs due to various causes. difference. As a result, the patient developed severe respiratory failure, unresponsive to high-dose oxygen.Patients with advanced respiratory distress syndrome are at high risk of complications:
Complications related to mechanical ventilation: Trauma, pneumonia; Other complications: Psychosis, deep vein thrombosis, peptic ulcer, malnutrition, catheter infection,...
2. Causes of progressive acute respiratory distress syndrome

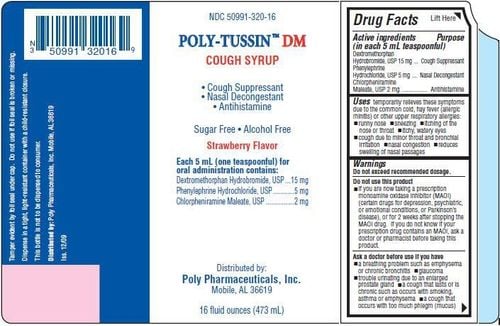
Viêm phổi nặng là nguyên nhân gây suy hô hấp cấp thường gặp nhất
2.1 Pulmonary causes Severe pneumonia: The most common cause Acute respiratory failure can appear after a patient has a bacterial pneumonia (pneumococcus, streptococcus, Haemophilus Influenzae, ... ) or viral pneumonia (influenza A H5N1, SARS,...);
Asphyxiation: Damage the surfactant membrane; Gastroesophageal reflux: Common in comatose or intoxicated patients. Gastric juice causes extensive lung damage with atelectasis; Injecting, snorting heroin or using other drugs such as cocaine, amphetamine,...; Pulmonary edema due to reperfusion after lung transplantation or pulmonary thromboembolism; Severe chest trauma causing contusion of the lung. 2.2 Extrapulmonary causes Severe infection or septic shock; Mass transfusion (> 15 units); Multiple fractures, head trauma, severe burns; Overdosing; Cardiopulmonary anastomosis; Disseminated intravascular coagulation; Severe acute pancreatitis.
3. Symptoms of acute respiratory failure
3.1 Clinical symptoms Rapid onset, usually within 4 - 48 hours after a cause of progressive pulmonary or systemic acute respiratory failure; Shortness of breath, bruised lips and extremities, rapid breathing; Auscultation of the lungs with diffuse crackles; rapid heart rate, rapid breathing, sweating; Contraction of accessory respiratory muscles; Cough, chest pain; Manifestations of the cause of acute respiratory failure such as fever, coagulopathy,... 3.2 Subclinical symptoms Blood gas tests: PaO2 decreased, often accompanied by decreased CO2, increased arterial-capillary oxygen gradient circuit; Chest X-ray: diffuse infiltrates of 2 lungs; Chest computed tomography: Image of diffuse infiltrative lesions of 2 lungs.
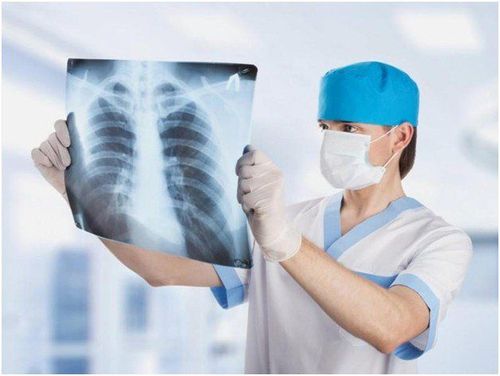
Hình ảnh X-quang phổi có thể có thâm nhiễm lan tỏa 2 phổi
4. Diagnosis of acute respiratory distress syndrome
4.1 Confirmation of diagnosis Advanced acute respiratory failure should be considered if the patient is at risk of illness such as asphyxia, coma (suspected aspiration of gastric services), pneumonia, malignant influenza, or clinical signs presumption of a progressive acute respiratory failure; Progressive acute respiratory failure is certain if the SaO2 and PaO2 tests are very low despite oxygen or IPPV ventilation; chest x-ray showed 2 lungs with fuzzy head or scattered cotton-shaped. 4.2 Differential diagnosis Due to the nonspecific symptoms of acute respiratory distress syndrome, doctors need to pay attention to distinguish it from different respiratory diseases, cardiovascular diseases, toxicities, infections,... Based on the patient's history, combined with a physical examination that focuses on the respiratory and cardiovascular systems, can help the physician narrow the differential diagnosis and determine the optimal course of treatment.
Need to differential diagnosis of acute respiratory distress syndrome with the following conditions:
Acute hemodynamic pulmonary edema : Due to acute left heart failure or acute fluid overload. Lesions on X-ray are butterfly-shaped, rapidly progressing and rapidly regressing; Diffuse alveolar hemorrhage: Respiratory failure with rapid blood loss, the patient coughs up bloody sputum, bronchoscopy has blood.
5. Treatment of acute respiratory distress syndrome
The principles of disease treatment are to identify and treat the causes, mechanical ventilation with lung protection, fluid balance, minimize complications, prevent complications and ensure proper nutrition suitable for the patient. Specifically:
5.1 Mechanical ventilation Objectives to be achieved are:
Blood oxygenation: Arterial blood gas with PaO2 55 - 80mmHg or SpO2 measurement of the fingertip is 88 - 95%; Plateau pressure (Pplateau) ≤ 30cm water; Arterial blood pH: 7.25 - 7.45. The doctor performs the setting of ventilator parameters to support the treatment of acute respiratory failure for each specific patient.
5.2 Sedation - muscle relaxant Use sedation or a combination of sedatives and muscle relaxants to ensure that the patient is fully mechanically ventilated (Ramsay score 4 - 5). However, sedatives - muscle relaxants need to be reduced in dose and stopped at the right time when the disease is getting better in order to stop mechanical ventilation in time, stop ventilator as soon as possible.
5.3 Ensure hemodynamics and fluid balance In essence, acute respiratory distress syndrome is a form of acute pulmonary edema. Therefore, the patient should not be given too much fluid too quickly. Do not give fluids and give the patient more than 1.5 liters of fluid/day.
Every day, medical staff should assess the fluid balance in - out in patients with advanced acute respiratory failure, ensure negative balance or zero. If the patient is gaining weight, the fluid balance is positive, need to use furosemide injection. IV at an appropriate dose to adjust to return the patient to baseline body weight and maintain a central venous pressure of 6 to 8 cm of water. Pulmonary capillary pressure is 8-10 mmHg (if Swan Ganz catheter is inserted).
5.4 Other treatments Use low doses of corticosteroids; Control blood glucose, if blood sugar > 10.0mmol/l, need to test capillary blood sugar at bed every 3 hours and use insulin to achieve blood sugar level 6-10mmol/l; Anti-infective antibiotic therapy: Immediately take antibiotics by de-escalation method, then adjust according to the antibiotic chart if any; In case of pneumonia caused by influenza A virus, it is necessary to follow a specific treatment regimen; Prophylaxis of thromboembolism: Use prophylactic dose of Heparin; Prophylaxis of peptic ulcers: Use a proton pump inhibitor, eg omeprazole; Measures to mobilize alveoli; Ensure adequate hemoglobin (>8g/l). 5.5 Monitoring and consolidation treatment After a few days of treatment, if progress is good, the patient will wake up, have a rosy face, and stable pulse and blood pressure.
The study of ventilator abandonment requires more caution than with other forms of acute respiratory failure, and intermediate measures such as spontaneous respiration with continuous positive pressure CPAP or forced artificial respiration with interruption should be used. interval IMV, SIMV (every 2-4 normal breaths, there is 1 forced breath of the machine).
5.6 Prophylaxis Actively treat pneumonia to prevent progression to acute respiratory distress syndrome; Keep the patient's head elevated, especially in those with impaired consciousness.
6. Progression and prognosis
Without proper treatment, patients with advanced respiratory failure will certainly die within hours to days. Manifestations are:
Consciousness disturbance leading to coma due to cerebral hypoxia; The pulse becomes faster, blood pressure drops, and then the pulse collapses; If the patient survives, the long-term prognosis is still difficult to assess, the patient may have pulmonary fibrosis, chronic respiratory failure, chronic bronchiectasis; The overall mortality rate is 50-70%. Mortality of the disease is mainly due to sepsis and non-pulmonary organ failure. Factors that increase the patient's risk of death are: advanced age, chronic liver disease, cirrhosis, alcoholism, sepsis, immunosuppression, chronic kidney disease, failure of any organ other than the lungs ,... Rehabilitation: Most patients with advanced respiratory distress syndrome will recover to near-normal lung function within 6 months. Acute respiratory distress syndrome has a high mortality rate. Early detection of the disease is important in improving the effectiveness of treatment. Therefore, when symptoms of acute respiratory failure develop, patients should quickly go to the doctor for timely diagnosis and treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.