This is an automatically translated article.
The article was professionally consulted by Doctor Tran Thi Diem Trang - Respiratory Internal Medicine Doctor - Department of Medical Examination & Internal Medicine - Vinmec Central Park International General Hospital.1. What is progressive acute respiratory failure?
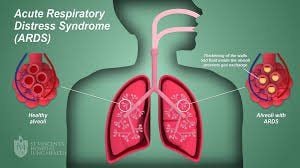
Adult acute respiratory distress syndrome (ARDS), first described in 1967, is a clinical syndrome with rapid onset of severe dyskinesia, hypoxemia, and diffuse pulmonary infiltrates leading to respiratory failure.
The cause of acute respiratory failure is due to a number of clinical disorders such as:
Severe pneumonia: The most common cause, bacterial pneumonia (eg, pneumococcal, streptococci, Influenzae.. .) or viral pneumonia (eg influenza A H5N1, H1N1, H7N9, SARS...). Asphyxiation: Damage to the sufartan membrane. Gastroesophageal reflux: Common in patients who are comatose or drunk, or have increased intracranial pressure, gastric juice causes extensive lung damage with atelectasis. Injecting, snorting Heroin or using other narcotic drugs (Cocaine, Amphetamine...). Severe chest trauma causing contusion of the lung. Severe infection or septic shock. Transfusion of large quantities (>15 units), especially whole blood. Severe acute pancreatitis; Acute kidney failure. Severe burns, especially respiratory burns.

2. Is progressive acute respiratory failure (ARDS) dangerous?
Incidence
The prevalence of ARDS is 58/100 000 person year with 141,500 new cases per year, annual mortality rate is 59,000 per year as reported in 2005 in US intensive care units. . Data from 2001-2008 suggest that rates of ALI and/or ARDS in hospitalized adult patients have decreased, perhaps due to widespread use of pulmonary protective ventilation, reductions in nosocomial infections, and use of blood products. more cautious.
Mortality rate
ARDS causes approximately 40% of deaths in 200,000 critically ill patients annually in the United States Pooled estimate of ARDS mortality from a systematic review is 36 - 44% with little change of more than two decade until 2006. Mortality rate decreased markedly in the studies from 1997 to 2009.
In Vietnam, there are no exact statistics but the mortality rate due to acute respiratory failure is also not small at all.
Advanced acute respiratory failure may have no initial symptoms or signs, so it is easy to miss. After 6 to 48 hours, the patient began to have more severe developments such as:
The patient's purple color is more obvious in the lips and extremities; Dyspnea increases and the lungs can be heard with moist crackles on both sides and a tube murmur can be heard. Chest X-ray will show clear alveolar and interstitial infiltrates. The thorax also shows extensive lesions on CT. Respiratory failure progresses rapidly and if the patient is not treated promptly, it can easily lead to death.
3. Treatment of advanced acute respiratory failure
Recently, the mortality rate of ARDS has improved significantly as a result of general progress in the care of critically ill patients. Therefore, care for patients with ARDS requires attention to (1) identification and treatment of underlying diseases; (2) Mechanical ventilation with lung protection mode; (3) Fluid balance (4) minimizing complications of treatment and procedures; (5) prevent venous thrombosis, gastrointestinal bleeding, aspiration, avoid excessive sedation, avoid infection (6) provide adequate nutrition.
Identify and treat causative diseases Identifying and treating causative diseases is very important in the management of ARDS. Only by eliminating the cause of ARDS can the patient emerge from respiratory failure.
Mechanical ventilation: Patients with severe ARDS with increased work of breathing and progressive hypoxia require mechanical ventilation. The requirement of mechanical ventilation is to ensure adequate arterial oxygenation and minimize the risk of ventilator-associated complications. Set breathing mode PCV or VPV. High frequency positive pressure ventilation (HFPPV). Extracorporeal membrane oxygenator (ECMO) circulation. Artificial ventilation with positive pressure both strokes and low frequency combined with a machine using a membrane to filter co2 out of the body.

Ensure hemodynamic and fluid balance: Infusion ARDS: There is no need to strictly limit water, but it should not be too fast and too much. In general, fluids and food should not be given more than 1 and a half liters a day. Weigh patient daily, assess fluid balance, ensure negative or zero balance. If the patient is gaining weight and fluid balance is positive, administer furosemide intravenously at an appropriate dose to adjust promptly to return the patient to baseline weight and maintain a central venous pressure of 6 to 8 cm of water. Pulmonary capillary pressure 8-10 mmHg (if Swan Ganz catheter is inserted). Other therapeutic measures: Corticosteroids: Many studies have studied corticosteroids in the treatment of both early and late ARDS to reduce inflammation in the lungs. Current evidence does not support the use of high-dose corticosteroids to treat ARDS,. However, there are specific situations where corticosteroids can be used with caution when the underlying cause responds to corticosteroid treatment (eg. such as cryptogenic organizing pneumonia). Control blood glucose: If blood sugar is > 10.0mmol/l, do capillary blood sugar test at bed every 3 hours and use insulin to get blood sugar level 6-10mmol/l. Anti-infective antibiotic therapy: Immediately take antibiotics by de-escalation method, then adjust according to the antibiotic chart (if any). In the case of pneumonia caused by influenza A virus (eg, H5N1), see the treatment regimen for influenza A pneumonia. Prophylaxis of thromboembolism: Use prophylactic doses of heparin. Gastrointestinal ulcer prophylaxis: Use a proton pump inhibitor (eg, omeprazole). Alveolar mobilization method: Refer to alveolar mobilization technique. Ensure adequate hemoglobin (>8g/l). After a few days, if progress is good, the patient will be awake, ruddy, blood pressure stable.
4. Prevention of acute respiratory failure
In order to effectively prevent acute respiratory distress syndrome, it is necessary to:
Treat diseases such as cardiovascular disease, chronic obstructive pulmonary disease (COPD), and prevent deep vein thrombosis of the lower extremities thoroughly. Avoid air pollution, toxic chemicals. Early antibiotic treatment is needed if bacterial pneumonia is suspected. Or, if viral pneumonia is suspected, it should be treated with antiviral drugs to avoid the disease progressing to advanced respiratory failure. ARDS is an important cause of acute respiratory failure, has a high mortality rate, is associated with many medical and surgical diseases. Although there is no specific treatment for ARDS yet, significant advances have been made in the treatment of patients with ARDS using strategies of lung-protective mechanical ventilation, fluid restriction, and management of myopathy. copy.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.