This is an automatically translated article.
The article is advised by Master, Doctor Nguyen Thi Nhat - Infectious Diseases - Department of Medical Examination & Internal Medicine - Vinmec Hai Phong International General HospitalIntravenous injection is a method of rapidly introducing drugs into the patient's body through a peripheral vein to bring about rapid systemic treatment.
1. Indications/contraindications for intravenous injection
Intravenous injection is a technique that uses a needle to put a drug into the body through a vein to quickly get an effect.
1.1 Indications for intravenous injection Emergency patients; The patient is exhausted; Severe patients need quick effects of drugs on the body: Anesthesia, sleep-inducing, anti-hemorrhagic, anti-vascular collapse,...; The drugs can cause necrosis of the skin, muscles, subcutaneous tissues, not absorbed or destroyed by the gastrointestinal tract; The drug has a systemic effect; It is necessary to put into the body a large amount of medicine; The drug is not injected intramuscularly or subcutaneously, only intravenously; Blood, plasma and colloidal solutions such as: Dextran, subtosan; Therapeutic serums; Patients who can't take medicine: Having a lot of vomiting, preparing for surgery, psychologically uncooperative.

Người bệnh bị nôn ói khi dùng thuốc sẽ được chỉ định tiêm tĩnh mạch
1.2 Contraindications for intravenous injection Oil-soluble drugs, rapid injections causing cardiac arrhythmias; Drugs causing strong stimulant to the cardiovascular system such as adrenaline (intravenous adrenaline only in case of emergency, when blood pressure drops, can't be measured, can't catch pulse,...) is absolutely contraindicated in intravenous injection in sites of infection, burns; Relative contraindications for intravenous administration in paralytic limb, edematous sites and joints. 1.3 Place of intravenous injection in the head: 2 sides of the temples; Veins of extremities: back of hand, wrist, elbow, instep, ankle,...; It is advisable to choose veins that are large, clear, and less mobile.

Vị trí tiêm tĩnh mạch
2. Intravenous injection technique
2.1 Nursing Preparation: Wash hands and dress appropriately; Patient and family: Explained how to administer intravenously, ask for allergy history, do antibiotic tests according to indications, assess vital signs; Prepare equipment: Includes sterile equipment (sterile tray, suitable syringe, pin, pin holder, cotton swab and cotton swab container), clean equipment (gloves, 70° alcohol, gauze cord, shockproof box) and medical records, waste buckets,...; Preparation of drugs: Injection, solvent, distilled water, 5% glucose when indicated for injection. 2.2 Intravenous injection procedure Administer intravenous injection according to the 5 right principles: Right patient, right drug, right route, right dose and right time. The procedure for intravenous injection is as follows:
Wash hands, disinfect hands, disinfect vial caps and solvents; Mix the drug, shake well, observe the color, properties, ... the drug, ensure good quality when used; Take medicine exactly as prescribed; Find a suitable injection site, tie a gauze if necessary, disinfect the injection site with a cotton swab soaked in 70° alcohol, let the skin dry; Insert the needle into the vein; Remove the gauze cord, inject the drug slowly, observe the patient closely during the injection process; Withdraw the needle quickly, tighten the skin and place the cotton in the injection site when the drug is out; Help the patient return to a comfortable position, guide the patient and family to monitor for abnormal signs of color, consciousness, respiratory status,...; Clean up equipment, wash hands, and record medical records. 2.3 Monitoring during and after intravenous injection Monitoring during injection: Observe the patient's face, if there are signs of anaphylaxis, quickly stop the injection, notify the doctor to handle the correct regimen. In addition, during the injection process, there may be some incidents such as needle blockage, swelling at the injection site, patient panic, etc., which should be promptly handled; Monitoring after injection: Monitor closely for late allergic reactions such as rash at the injection site or on the whole body.

Theo dõi sau tiêm tĩnh mạch, đề phòng phản ứng dị ứng muộn
2.4 Accidents and treatment when giving intravenous injection Needle blockage: Because the blood flowing into the needle is coagulated right at the tip of the needle, the drug cannot be injected. Treatment is by withdrawing the needle from the injection site, pushing the syringe to allow blood to flow out and if not, changing the needle; Injection site swelling: Due to the needle piercing the vessel or the bevel of the needle, half is inside the vessel and half is outside the vessel. To treat, it is necessary to withdraw the needle and inject again. After the injection is complete, apply hot compresses to the swelling to dissolve the hematoma and help the drug dissolve quickly; Embolism: Due to the presence of air in the syringe into the vessel or the wrong injection of a fat-soluble, milky drug. To prevent the risk of embolism, it is advisable to clear the air in the syringe before injecting the patient and to avoid misusing the drug; Patients with fainting, panic: Should do a good job of patient psychology before intravenous injection. If the patient is shocked or fainted due to fear or drug reaction, the injection is too fast, the needle is punctured many times without hitting the vein, etc., the injection should be stopped and reported to the doctor for treatment; Infection: Due to poor sterility or prolonged retention of needles. Measures to prevent the risk of infection is to perform aseptic work well before, during and after injection for the patient, and at the same time keep in mind the time of needle retention; Necrosis: Due to out-of-venous injection of drugs that are contraindicated for subcutaneous and intramuscular injection. Manifestations are injection site hot, red, painful, initially hard, then soft. The appropriate treatment is hot compress, when there is necrosis, the bandage should be thin, not to cause further infection and if the necrosis is large, it is necessary to make an incision; Anaphylaxis: Due to the body's reaction to the drug used. Manifestations of anaphylaxis are restlessness, fear, lethargy or coma, rapid, small pulse, shortness of breath, cyanosis, rash, erythema, allergic urticaria,... Measures to manage are immediately stop injection and properly handle anaphylaxis emergency protocol; HBV, HCV, HIV infection: HBV, HCV infection caused by sterile needles and syringes causes the virus to be transmitted from hepatitis patients to healthy people (detected 4-6 months after injection with symptoms including fatigue, jaundice, yellow eyes, loss of appetite, dark urine) and HIV infection due to intravenous injection do not ensure the principle of aseptic. The treatment will be prescribed by the doctor on a case-by-case basis.

Tiêm tĩnh mạch có thể gặp một số tai biến
3. Intravenous infusion technique with locking needle
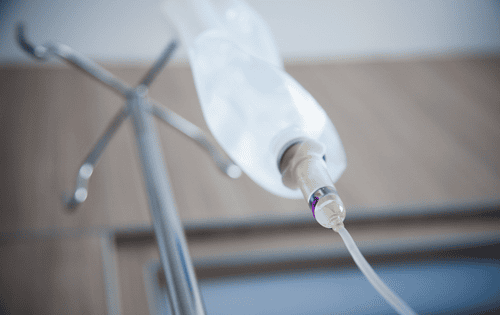
The technique of intravenous infusion with a catheter needle is a method of injecting, intravenous infusion using a needle with a soft plastic tube inserted into the vein, firmly fixed into the vein, the needle tip is not sharp, so there is no ability to penetrate the vessel wall.
This technique is used in cases where the patient is indicated to have injections or infusions several times a day or to maintain injections or infusions for many days. Peripheral vein catheter needles overcome the disadvantages of iron needles such as causing venous deviation, transvascularization, pain during infusion.
3.1 Indications / contraindications Indications
Patients need emergency resuscitation: Shock, pulse collapse, coma, respiratory failure, circulatory arrest,...; Continuous infusion; Intermittent infusion; Intravenous injection and infusion of drugs; Transfusion of blood, blood products; Before performing procedures, surgery or using contrast agents,...; In case of short-term intravenous nutrition, Contraindications
Venous area damaged, infected, bruised, burned,...
Bệnh nhân cần truyền dịch liên tục
3.2 Implementation of the technique Inform and explain the technique to the patient and the patient's family; Ask for a history of drug allergies; Nurses wear masks, wash hands quickly; Prepare the same device for intravenous injection; Check rule 5 true; Put the patient in a suitable position, expose the injection site; Disinfect hands, wear clean gloves, disinfect needle lock; Check the catheter, perform drug injection; Rinse the retainer by injecting saline; Withdraw the needle, use a cotton pad to wipe the lock, apply gauze to cover the needle tip; Instruct patients and family members on how to monitor after intravenous infusion; Clean tools and record medical records.

Truyền tĩnh mạch có khóa lưu kim
3.3 Follow-up Track the patient's facial expression and evolution during and after the technique; Care of the catheter needle every 8 - 12 hours or depending on the actual condition of the patient; Check the needle placement area daily; Catheter needles should not be left for more than 3 days; When there are signs such as needle blockage, swelling, redness, pain along the vein, local bleeding, or infection, the needle should be removed and the needle placed in another position. 3.4 Accidents and treatment Accidental puncture of the artery: Need to immediately withdraw the needle, apply pressure at the point of needle insertion and monitor for signs of local bleeding to handle the next steps accordingly; Extravasation: Due to needle deviation, vein rupture, need to withdraw the needle, change the IV infusion site to another limb and regularly check and report to the doctor for proper treatment; Hematoma : Due to bleeding into the surrounding tissue or the needle passing through a blood vessel. Treatment is to remove the needle and apply cold compresses around the site of hematoma; Loss of catheter: Because the catheter is not fixed securely or the patient withdraws the infusion on their own, it should be handled by withdrawing the infusion needle; Phlebitis : Due to the appearance of blood clots at the tip of the catheter needle, keeping the catheter needle for too long, the infusion solution has a pH that is too high or too low. The treatment is to remove the needle, apply heat and notify the doctor for appropriate changes; Local infection: Treat by withdrawing the needle, changing the intravenous infusion site to another limb, informing the treating doctor and monitoring and taking care of the infection site according to the protocol; Systemic infections: Due to poor aseptic practice, poor intravenous care, long-lasting catheter needle retention, prolonged phlebitis or immunocompromised patients. In this case, it is necessary to inform the doctor to use the drug according to the indications and monitor the vital signs as well as the patient's general condition; Other complications: Venous spasms, circulatory overload, drug allergies, ligament damage, nerve damage, gas embolism, ... perform proper treatment according to the treatment protocol as directed. guide.

Sau tiêm truyền tĩnh mạch có khóa lưu kim, người bệnh cần được theo dõi vị trí lưu kim
4. Some important notes when administering intravenous infusion using a needle lock
Use sterile gauze to cover the catheter site; Change bandages, gauze every 24 - 48 hours or change immediately when the bandage, gauze is semi-absorbent, not guaranteed to be intact; It is necessary to change the position of the catheter every 48 - 72 hours, if it is not possible to change the position of the infusion needle, it is necessary to notify the doctor for appropriate treatment; If not in use, the catheter should be removed immediately. When being assigned to perform intravenous injection, patients need to coordinate with medical staff to ensure the best treatment effect.
MORE:
What are peripheral vascular diseases? Causes and warning symptoms What does the cold say about your health? Guidelines for prevention and care of people with varicose veins