This is an automatically translated article.
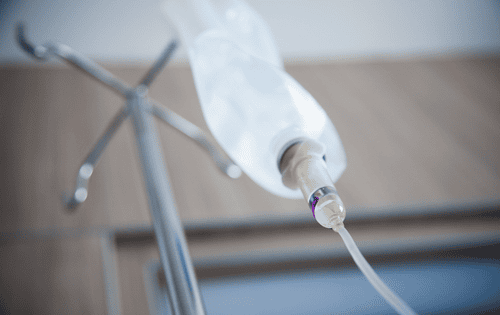
The article is advised by Master, Doctor Nguyen Thi Nhat - Infectious Diseases - Department of Medical Examination & Internal Medicine - Vinmec Hai Phong International General HospitalIntravenous infusion is the method many people choose to put in a possible amount of water, nutrients ... to supplement nutrients for the body. However, if not done properly and really necessary, it can cause some complications such as acute pulmonary edema, hypertension, acute heart failure.
1. Overview of infusion therapy
Infusion therapy is a form of introducing large amounts of water, nutrients, and electrolytes into the body. There are 2 ways to infuse the solution into the patient's body:
Intravenous infusion: Usually in a peripheral vein or in the center Subcutaneous infusion: Only applicable to a limited number of specific solutions. Although the infusion technique is quite simple, if done incorrectly, it is also easy to have complications such as: stroke, metabolic disorder, anaphylaxis (due to too fast infusion rate), edema in the heart, kidneys , the patient's body is allergic to the components of the infusion... Even infusion can infect chronic diseases such as hepatitis, HIV.
Infusion is a soluble solution containing many different ingredients, which can be injected under the skin or directly intravenously from the patient. Most of the solvents used are distilled water or some other solvent is used to dissolve the drug.
Currently there are about 20 types of infusion fluids and patients need to perform tests to determine exactly which type of fluid needs infusion, the appropriate dosage to use to avoid unfortunate complications.
Infusion fluids are divided into 3 basic groups as follows:
Supplementing nutrients for the body: Including glucose 5%, 10%, 20%, 30% and solutions containing vitamins, proteins, substances fat. Replenish water and electrolytes: Including lactate ringer solutions, sodium bicarbonate 1.4%, sodium chloride 0.9%... used in case of dehydration, blood loss. Albumin compensation: Special solutions such as fresh plasma, albumin-containing solutions, dextran solutions, gelofusine, haes-steril or macromolecular solutions... are used in case of need for rapid replacement of albumin or weekly volume. complete in the body.
Dịch truyền vào cơ thể có nhiều loại khác nhau
2. When should intravenous infusion be given?
As recommended by many doctors, infusion therapy should only be applied in cases where it is absolutely necessary, avoiding self-infusion without a doctor's appointment.
In some cases, intravenous infusion should be given, including:
The patient has a high fever, vomiting a lot causing dehydration, diarrhea, low blood pressure ... difficult to eat. If the patient is dehydrated but still able to eat and drink, oral rehydration will be more effective than intravenous fluids. People who are weak, eat poorly, have severe vitamin deficiencies, or have an imbalanced body can infuse a solution containing multivitamins (fruit juice) to improve their health and help them eat better. On the contrary, if healthy people drink fruit juice, it can lead to anorexia, even edema of the heart and kidneys because suddenly a large amount of water and nutrients are introduced into the body. In contrast, intravenous fluid administration is contraindicated when:
Patients with severe heart failure Patients with hypertension Healthy people do not necessarily need fluids If there are special indications such as need to maintain a certain amount of fluid In the blood, it must be infused very slowly, with a small volume combined with close monitoring, and measurement of central venous pressure.

Bệnh nhân tăng huyết áp không nên truyền tĩnh mạch
3. Intravenous infusion procedure
Before performing intravenous infusion, the patient should defecate, urinate to prepare for a long time of infusion.
Step 1: Medical staff will read the label and check the infusion bottle, confirm information such as the name of the fluid, quantity, quality, and expiry date. Use a marker to write all information on the bottle body.
Step 2: Then attach the hanging cage (if necessary) and open the cap of the infusion bottle. Insert the end of the infusion line into the bottle, expel the air by locking the stopper.
Step 3: Squeeze the rubber tip for the liquid to run down 1/2 cup of the bottle. Unlock the fluid to slowly flow into the pea tank until the wiring is no longer air, then lock the lock. Add medicine to the infusion bottle (if necessary).
Step 4: The medical staff instructs the patient to lie in an appropriate position to reveal the injection site. Should choose the injection site in a straight, large, less mobile vein.
Step 5: Put a small pillow or small rubber sheet under the injection area (if necessary), then tie a tourniquet 7-10cm from the injection area, ask the patient to make a fist.
Step 6: Disinfect the injection area in a spiral from the inside to the 5cm wide with an antiseptic solution.
Step 7: The medical staff uses the right hand to hold the needle and insert it into the vein at an angle of 15-30 degrees from the skin surface, then lower the needle and thread it up along the vein into 2/3 of the needle's length. One hand holds the needle, the other hand squeezes the soft rubber part of the infusion line to see if there is any bleeding or not, if it is correct. If there is no blood, adjust the needle until it enters the correct vein.
Step 8: Open the tourniquet, unlock the fluid to flow into the vein, tell the patient to let go. At the same time, advise the patient the necessary things:
If the fluid does not flow, immediately notify the medical staff. When the infusion is over, notify the medical staff immediately. The patient does not arbitrarily unlock the infusion bottle to make the water flow faster. Do not move where the transmission site is too strong. If the injection site is edematous, painful, or has strange reactions such as cold shivering, fatigue, shortness of breath, etc., it is necessary to notify the medical staff. In addition, during intravenous infusion, medical staff must visit the patient every 30 minutes to detect complications during the infusion.
When the bottle is about 15-20ml almost empty, lock it, remove the tape and remove the needle. Use a cotton swab soaked in alcohol to press on the injection area (or if infusion, change the bottle). Carefully clean the medical equipment after the infusion is completed.

Truyền dịch vào tĩnh mạch
4. Attention when giving intravenous fluids
Notes when performing infusion therapy for patients:
Infusion fluid and tools used must be absolutely sterile Make sure to practice the correct procedure and technique for infusion during the injection process Absolutely do not allow air to enter the vein and ensure that the pressure of the infusion is higher than the patient's venous blood pressure. Medical staff should closely monitor the patient's condition before, during and after the infusion to detect and handle reactions early (if any). The point of contact between the needle and the skin surface must be kept absolutely sterile. When the body is weak, anorexia, the patient needs to review his diet, sleep, work and exercise accordingly. In the case of still eating and drinking, instead of infusion should be supplemented with fish, meat, eggs, milk... it will be more effective and safer than infusion During the infusion, if the body has symptoms abnormal symptoms such as chills, shortness of breath, swelling at the injection site, etc., must be reported immediately to medical staff for timely treatment, to avoid more dangerous reactions Intravenous infusion procedures must be carried out in medical facilities that are qualified and capable of handling complications during infusion, limit infusion at home, on the road, on vehicles At medical facilities, emergency drugs should be available. Shock, shock to prevent unfortunate cases can still timely save patients

Khi sức khỏe có dấu hiệu bất thường, người bệnh nên đến cơ sở y tế để được thăm khám
To register for examination and treatment at Vinmec International General Hospital, you can contact Vinmec Health System nationwide, or register online HERE
SEE MORE
Dangers of self-infusion What does infusion (protein) do to the body? Infusion when dengue fever: Do not arbitrarily