This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General HospitalOn January 5, 2020, WHO issued a global warning after 44 patients were hospitalized with pneumonia of unknown cause, reported by the Chinese national authorities. On March 11, 2020, WHO declared a new coronavirus, identified as coronavirus 2, causing severe acute respiratory syndrome (SARS-CoV-2) and causing the so-called coronavirus disease 2019 (COVID-19). ), is a pandemic.
To date (January 2021), SARS-CoV-2 infection is approaching 100 million cases worldwide, while 2 million related deaths have been reported globally.
1. Characteristics of SARS-CoV-2
SARS-CoV-2 is a virus of the genus Betacoronavirus, family Coronaviridae, subgenus Sarbecovirus, discovered in late 2019. It is a positive-sense, single-stranded RNA virus with a diameter of 50-200 nm. . Because of its close genetic similarity to the bat coronavirus, an animal origin has been suggested based on animal-to-human transmission. SARS-CoV-2 possesses four structural proteins known as S (spiky), E (enveloping), M (membrane) and N (nucleocapsid) proteins; protein N binds to the viral genome while S, E and M proteins contribute to the assembly of the viral envelope Respiratory impairment is the most frequent clinical concern during this new viral infection; however, other physiological organ systems may be affected. In this article, the hepatic changes caused by SARS-CoV-2 are of interest because of their possible relationship with the liver and patient outcomes.
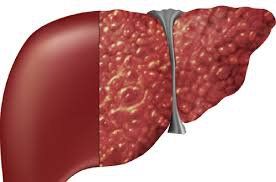
2. The liver plays a fundamental role in the metabolism and synthesis of plasma proteins
The liver plays a fundamental role in the metabolism and synthesis of plasma proteins, as well as in the regulation and detoxification of dietary xenobiotics. Several conditions can lead to chronic hepatitis and cirrhosis or hepatocellular carcinoma, including viral agents, alcohol abuse, metabolic disorders, and others. Patients affected by liver disease are fragile, and the patient's clinical stability is in perennial equilibrium. Among the direct causes of hepatic decompensation, the deleterious effects of infections, both viral and bacterial, are well known, and in this particular context, COVID-19 appears to be no less important. This review summarizes the effects of SARS-CoV-2 infection in normal tissue and normal liver.
Tác động có hại từ COVID-19 có thể gây mất bù ở gan
3. Interaction of SARS-COV-2 with normal tissue
The SARS-CoV-2 molecular pathways that the virus uses to facilitate host interaction and entry are of primary concern. Several studies have been performed in this regard, and much of the evidence converges to identify angiotensin-converting enzyme 2 (ACE2), a surface peptidase responsible for blood pressure regulation, as the key factor. In fact, Zhou et al. demonstrated that ACE2 is the major entry pathway of SARS-CoV-2 in cells, as was previously observed for SARS-CoV and HCoV-NL6 viruses. During the previous SARS pandemic in 2003, it was demonstrated that the administration of antibodies against ACE2 effectively counteracted viral replication. On the other hand, ACE1 antibodies do not have any effect. The interaction between this new virus and ACE2 was also investigated in a study conducted by Xu et al, where a strong association between the virus and this receptor was confirmed. ACE2 is present in various organs and tissues, such as type 2 alveolar cells of the lung; epithelial cells of the nasal mucosa, nasopharynx and mouth; in the smooth muscle of the gastric mucosa and colon; in the enterocytes of the duodenum, jejunum, ileum and colon; in cardiomyocytes; in the cells of the proximal tubules of the kidney; and in bile cells in the liver.
4. Any tissue expressing ACE2 can be a target of SARS-CoV-2
From all of the above, it is clear that any tissue that expresses ACE2 can be a target of SARS-CoV-2, giving rise to different symptoms with possible severity as to organ function. basic reserve. Major organs expressing ACE2 with corresponding symptoms/complications associated with COVID-19, are reported in Figure 1. Although the main clinical presentation is a mild flu-like syndrome, severe bilateral interstitial pneumonia leading to acute respiratory distress syndrome (ARDS) and requiring the intensive care unit (ICU) is not uncommon. Other common clinical manifestations include: Nausea, vomiting, anorexia, diarrhea (2%-10% of patients), and altered liver function tests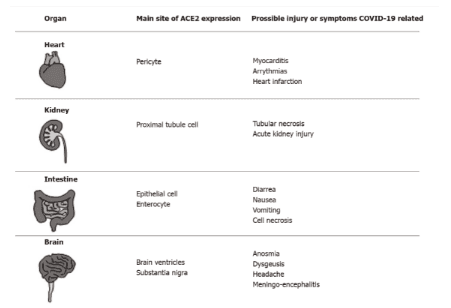
5. COVID-19 and normal liver
A large retrospective study, conducted in New York City, enrolled approximately 5700 COVID-19 patients. Liver transaminase levels were assessed on admission. Elevated aspartate transaminase (AST) or alanine transaminase (ALT) was found in 58% and 39% of patients, respectively. Worsening of the disease during hospital stay was associated with further increases in these enzymes. However, the pathogenesis of these changes remains unclear. In fact, several factors may have contributed to the liver changes in this heterogeneous group of patients, such as: (1) direct cytotoxic effects of the virus; (2) activation of the cytokine cascade; (3) onset of multiple organ failure; (4) disseminated intravascular coagulation; and (5) the use of potentially hepatotoxic drugs (such as remdesivir), among others. As demonstrated by other research, during COVID-19 administration, elevations in liver enzymes are characterized by an increase in AST preferentially, thus recalling the picture observed in alcoholics, transitioning metabolism or ischemia in the liver. Abnormal levels of cholestatic markers were rarely observed, even when elevated gamma-glutamyltransferase (GGT) levels were reported in 50% of patients in one study.
6. The onset of circulatory failure may reasonably explain the biochemical pattern of AST, ALT, and GGT changes.
Although SARS-CoV-2 virus particles have been described in hepatocytes in two severe cases, direct cytotoxic effects do not seem to explain changes in the liver because ACE2 mainly expresses present in the biliary tract and in the liver. On the other hand, despite: (1) the presence of receptors on bile cells; and (2) “in vitro” evidence of tight junction injury and impaired bile acid transporter in these cells; Cholestasis is rarely observed in the clinical setting of COVID-19. Regarding liver injury, however, it is important to emphasize that cardiomyopathy, with consequent myocardial dysfunction, is observed in nearly 33% of hospitalized COVID-19 patients. In this context, the onset of circulatory failure could reasonably explain the biochemical pattern of AST, ALT, and GGT changes, as in the more common picture of congestive liver disease. Supporting this view, a postmortem analysis of liver tissue from COVID-19 patients revealed a necrotic lesion associated with hypoperfusion and congestive changes. Finally, even if liver involvement is not generally considered relevant in subjects without pre-existing hepatic impairment, assessment of liver changes during COVID-19 remains challenging in the context of clinical situation, due to a lack of clear understanding of this process. In view of this, elevated bilirubin, even when rarely observed, seems to put patients at increased risk of mechanical ventilation or death compared with changes in other liver enzymes.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.