This is an automatically translated article.
Middle East respiratory syndrome (MERS) is a respiratory illness caused by a new type of coronavirus. This virus has many different strains that cause illnesses ranging from the common cold to severe acute respiratory distress syndrome (SARS). The following is the latest information from the World Health Organization on the disease caused by the MERS CoV virus.1. What is Middle East Respiratory Syndrome (MERS)?
Middle East respiratory syndrome (English name is Middle East respiratory syndrome and abbreviated as MERS) is a respiratory disease caused by a coronavirus virus (Middle East respiratory syndrome coronavirus, or MERS CoV) was first identified. discovered in Saudi Arabia in 2012. Coronaviruses have many different strains that cause illness in humans, from the common cold to severe acute respiratory distress syndrome (SARS). An estimated 35% of patients infected with MERS-CoV have died.2. Where was the MERS virus found?
Since 2012, MERS has been reported in 27 countries worldwide with approximately 80% of human cases reported by the Kingdom of Saudi Arabia. The cases identified outside the Middle East are people who were infected in the Middle East and traveled to other countries.3. How is the MERS virus transmitted?
The MERS virus is transmitted primarily from animals to humans, but can also be transmitted from person to person.From animals to humans MERS-CoV is a transmissible virus, which means it is transmitted between animals and people. Scientific evidence suggests that humans become infected through direct or indirect contact with infected camels. The MERS virus (written as MERS-CoV) has been found in camels in several countries, including Egypt, Oman, Qatar, and Saudi Arabia. In addition, there is ample evidence that MERS-CoV can spread to camels in the Middle East, Africa and parts of South Asia. Other animals can also be vectors, but animals such as goats, cows, sheep, buffaloes, pigs and wild birds are not hosts for this virus.
Person-to-person transmission MERS-CoV is not easily transmitted between people, unless there is close contact, such as health care workers treating and caring for an infected patient without taking precautions. strict household. Meanwhile, the majority of MERS cases reported to date have occurred in healthcare settings, so no human-to-human transmission has been detected in the country to date. anywhere in the world.
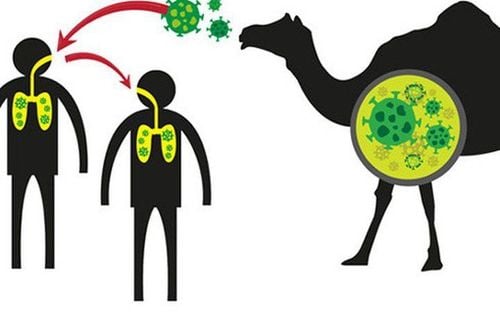
Virus MERS được truyền chủ yếu từ động vật sang người, nhưng cũng có thể truyền từ người sang người
4. What are the symptoms of MERS?
Typical symptoms of MERS include fever, cough, and/or difficulty breathing. Pneumonia is a common symptom, but some people infected with the MERS virus have no symptoms. Gastrointestinal symptoms, such as diarrhea, are also found in some patients. Severe cases can lead to respiratory failure and require mechanical ventilation in the intensive care unit or intensive care unit.Some patients have had organ failure, especially kidney failure or septic shock. This virus causes more severe illness in people with weakened immune systems, the elderly, and people with chronic conditions such as kidney disease, diabetes, cancer, and chronic lung disease. The mortality rate among people infected with the MERS virus is around 35%, however this number may be overestimated because mild cases can be overlooked.
5. Is there currently a vaccine for MERS CoV?
There is currently no vaccine or specific treatment for MERS, but scientists are continuing to develop a number of vaccines against the disease caused by the MERS virus. The main treatment regimen is supportive treatment based on the clinical condition of each patient.6. Is it easy to detect people infected with MERS-CoV?

Triệu chứng ban đầu của MERS thường dễ nhầm lẫn với viêm đường hô hấp cấp tính
7. What should be done when coming into contact with someone who has MERS?
If you have had close contact with someone infected with MERS-CoV within the past 14 days without using recommended infection control precautions, you should seek medical attention as soon as possible for a diagnosis. Soon.8. Should contact with camels or camel products be avoided?

Bất cứ ai tiếp xúc với trang trại, chợ, chuồng nên rửa tay trước và sau khi chạm vào động vật
Consumption of raw or undercooked animal products, including milk and meat, carries a high risk of infection from a variety of microorganisms. Animal products that have been cooked or pasteurized are safe to use, but consumers should also be careful to avoid cross-contamination with undercooked food. Camel meat and camel milk are nutritious products that can be used after pasteurization, cooking or other heat treatment.
Until more is understood about MERS-CoV, people with diabetes, kidney failure, chronic lung disease, and immunocompromised individuals are at increased risk for severe illness from MERS-CoV infection. . Especially in the Middle East, this group of people should avoid contact with camels, drink camel milk or camel urine, and should not eat undercooked meat.
Camel farms and slaughterhouse workers should practice good personal hygiene, including frequent hand washing, face protection and wearing protective clothing. After use, protective equipment should be removed immediately and cleaned daily. Workers should also avoid allowing household members to come into contact with clothing, shoes, or work items that have come into contact with camels or camel secretions. Sick animals should be culled and should not be slaughtered for consumption.
Source: WHO
See more:
2019-nCoV is similar to the virus that causes MERS and SARS? Guidelines for diagnosis and treatment of acute pneumonia caused by new Corona virus of the Ministry of Health To prevent 2019-nCoV, do I have to wear a mask continuously? What is the correct way to wear a mask?