This is an automatically translated article.
Posted by Master, Doctor Mai Vien Phuong - Department of Examination & Internal Medicine - Vinmec Central Park International General Hospital
Although the basic treatment of ulcerative colitis is medical, about 20 - 30% of patients require surgery. Indications for surgery are divided into three categories: emergency, delayed, and elective.
1. Principles of treatment and assessment of treatment response
The choice of treatment modality depends on the severity and extent of the lesion and the individual characteristics of each patient such as frequency of recurrence, course of disease, response to previous treatments, effects of side during treatment. Age of onset, extra-gastrointestinal manifestations, and duration of disease are also important factors. The sum of these factors helps to group patients into patients with severe disease requiring inpatient treatment and patients with mild to moderate disease who can be managed as an outpatient. Use of the Truelove and Witts classification in clinical practice has been proven and is now a widely used indicator. In some settings, erythrocyte sedimentation rate > 30 mm/hr can be replaced by a CRP > 30 mg/l. To assess disease activity, some guidelines for the use of the Mayo-scale have been developed based on the frequency of bowel movements, rectal bleeding, endoscopic imaging, and general evaluation in which, if no results are obtained, Endoscopic findings, using an inadequate Mayo score are still of clinical significance. During follow-up, the definition of treatment response, remission as well as resistance is important in optimizing and modifying treatment regimens. The 2015 Toronto Consensus provided definitions for these situations.Definition of treatment response levels according to the Toronto consensus
| Khái niệm | Định nghĩa |
| Hồi phục hoàn toàn | Tất cả các triệu chứng trên lâm sàng và tổn thương trên nội soi đều hồi phục. |
| Hồi phục tồn thương trên nội soi | Niêm mạc bình thường hoặc mạng lưới mao mạch không rõ, có thể có biến đổi mạn tính (polyp viêm, sẹo) nhưng niêm mạc không dễ chảy máu. |
| Lui bệnh về triệu chứng lâm sàng | Số lần đại tiện bình thường (<3 lần/ngày), phân không có máu. |
| Đáp ứng về triệu chứng lâm sàng | Có sự cải thiện về triệu chứng lâm sàng do chính bệnh nhân và bác sĩ đánh giá, có thể coi là tiêu chí đánh giá đáp ứng điều trị sớm. |
Toronto consensus definition of treatment failure
| Khái niệm | Định nghĩa |
| Thất bại với thiopurine | Bệnh nhân không duy trì được sự lui bệnh hoàn toàn khi không sử dụng corticosteroid mặc dù đã tối ưu hóa liều điều trị |
| Thất bại với chế phẩm sinh học |
-Thất bại nguyên phát: Bệnh nhân không đạt được lui bệnh hoàn toàn khi không sử dụng corticosteroid mặc dù đã tối ưu hóa liều điều trị -Thất bại thứ phát: Bệnh nhân không duy trì được lui bệnh hoàn toàn khi không sử dụng Corticosteroid sau khi đạt được đáp ứng về TCLS |
2. Indications for surgery
Although the basic treatment of ulcerative colitis is medical, about 20 - 30% of patients require surgery. Indications for surgery are divided into three categories: emergency, delayed, and elective.
Indications for emergency surgery are set out for patients with life-threatening complications of fulminant colitis, unresponsive to medical treatment.
Indications for delayed surgery are made for critically ill patients who do not respond to medical treatment.
Cases with long-term progression of disease with many relapses or intolerance to drugs, presence of dysplastic lesions or colorectal cancer will be in the elective surgery group.
Selection of surgical method depends on indications for emergency/delayed/selective surgery, patient's comorbidities and surgeon's experience. The goal of emergency surgery is resection of the inflamed colon, and sacral reconstruction should be avoided in emergency surgery because of the risk of bleeding, infection, or damage to the iliac nerve. After the patient has fully recovered, an ideal-pouch analanastomosis (IPAA) and an ostomy can be performed to minimize the risk of complications.
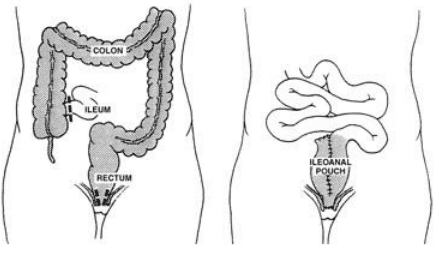
Total colectomy and IPAA ileostomy.
According to ECCO recommendations, delaying surgery in cases where it is indicated increases the risk of complications. For patients with acute colitis treated with > 20 mg of prednisolone/day for more than 6 weeks or for patients on anti-TNF therapy, a biphasic surgery may be an option. Then the first part of the colectomy and temporary ileostomy to reduce inflammation. After improving the new state of the body, the next step is to create an IPAA or make a permanent artificial anus. In large centers with good surgeon experience, laparoscopic surgery may be an option in cases of nontoxic colitis. Results in a review study showed that laparoscopic surgery in this group of patients had a lower rate of infection, abdominal abscess and shorter hospital stay. The most common complication after total colectomy and IPAA reconstruction is sacroiliitis. This is a non-specific inflammation of the ileal mucosa remaining after surgery and the incidence can be up to 50% within 10 years. Symptoms of pouchitis include: Increased frequency and volume of daily bowel movements, looser stools, and abdominal pain. Occasionally, bloody stools, fever, fecal incontinence, or extra-gastrointestinal symptoms may occur. Risk factors for pouchitis include generalized hemorrhagic ulcerative colitis, presence of primary sclerosing cholangitis, positive PANCA antibodies, and NSAID use. Depending on the course, activity level and frequency of inflammatory episodes in a year, pouchitis can be divided into types: Primary or secondary, stable or active, frequent (>3 times) /year) or rarely. In addition, based on the level of response to antibiotic treatment, it can be divided into three types: response to antibiotic treatment, antibiotic-dependent or treatment-resistant. Complications of sacroiliitis include abscesses, fistulas, narrowing of the anastomosis, and presence of cancerous lesions. Malignant progression occurs almost exclusively when a previous colectomy specimen contains dysplastic or cancerous lesions.
According to ECCO, treatment of complications of pouchitis, using antibiotics metronidazole or ciprofloxacin. In addition, anti-diarrheal drugs can be combined to reduce the number of bowel movements. About 10 - 15% of patients with acute pouchitis will progress to chronic, of which some may respond, some develop resistance to an antibiotic during treatment. Therefore, these cases require a combination of two antibiotics. Budesonide, oral beclomethasone dipropionate have also demonstrated efficacy and may be alternatives. Patients with persistently refractory chronic pouchitis can benefit from biologics such as infliximab. In case of resistance to infliximab can choose adalimumab instead.
Surgical indications at Vinmec International General Hospital are performed by a team of well-trained and experienced doctors and nurses, with the support of a system of modern equipment to help minimize the risk. the risk of complications after surgery, bringing health and peace of mind to the patient.
Patients who visit and undergo surgical treatment at Vinmec will enjoy the following benefits:
Consult and agree on a treatment plan throughout from a team of doctors from many specialties; The development of an optimal treatment regimen helps patients avoid having to test different treatment methods, which is costly, time consuming and affects the overall treatment effectiveness; Patients can better manage costs thanks to a one-time payment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Articles refer to the source: BARGENJ (1929). Complications and sequelae of chronic ulcerative colitis*. Annals of Internal Medicine, Basler RW and Dubin HV (1976). Ulcerative colitis and the skin, Lichtenstein G.R., btv. (2014), Medical Therapy of Ulcerative Colitis, Springer-Verlag, New York