This is an automatically translated article.
The article is professionally consulted by Master, Doctor Tong Van Hoan - Emergency Medicine Doctor - Emergency Department - Vinmec Danang International Hospital. Doctor with 10 years of experience in the field of Emergency Resuscitation.BiPAP non-invasive artificial ventilation is a method of breathing support for patients with problems in the heart, lungs,... This method of artificial ventilation is indicated, contraindicated for each specific case. .
1. What is BiPAP Non-Invasive Artificial Ventilation?
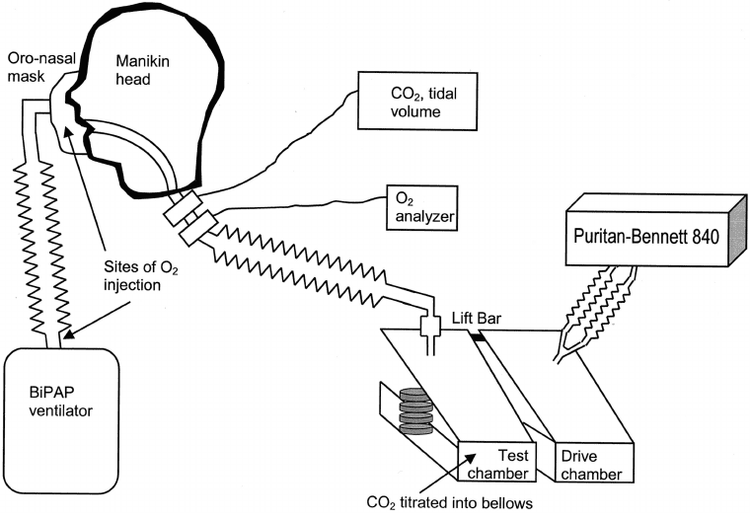
Patients who cannot breathe spontaneously can use artificial ventilation. Artificial ventilation includes non-invasive ventilation and invasive ventilation. Non-invasive ventilation is a method that does not use an endotracheal tube or tracheostomy.BiPAP (bilevel positive airway pressure) is a non-invasive artificial ventilation method that partially supports the patient's natural respiration with 2 levels of continuous positive pressure in the airways including:
IPAP: Positive pressure Inhale, equivalent to PSV; EPAP: Positive expiratory pressure, equivalent to PEEP; The purpose of this method of artificial ventilation is to:
Reduce mean and peak pressures in the airways, reduce complications of hypertension and chest tightness for the patient; Reduces expiratory flow resistance, reduces respiratory work for the patient, helps oxygenate the blood, and avoids the risk of atelectasis.
2. Indications/contraindications for BiPAP . non-invasive artificial ventilation
2.1 Indications Respiratory support in cases of respiratory failure but still breathing. Specifically:After surgical anesthesia; After cardiopulmonary surgery; Mild severity of exacerbation of chronic obstructive pulmonary disease, acute lung injury, progressive acute respiratory failure, acute pulmonary edema; Heart failure ; Have sleep apnea syndrome; After extubation of the endotracheal tube; Premature infants: With endocardial disease, apnea, bronchopulmonary dysplasia, mild-moderate meconium aspiration syndrome, pulmonary edema, pulmonary bleeding, delayed pulmonary drainage, laryngospasm, molluscum contagiosum management, pulmonary hypertension, weaning off ventilators for pediatric patients requiring prolonged invasive ventilation or extremely premature babies.

3. Perform BiPAP . non-invasive artificial ventilation technique
3.1 Preparation of Executors: Doctors and nurses specializing in Emergency Resuscitation; Equipment - facilities: Ventilator with BiPAP breathing method, non-invasive breathing mask, sterile plastic ventilator airway set, common sputum suction catheter, closed sputum suction catheter, oxygen system, compressed air system, suction system, blood gas testing machine, continuous monitoring machine (electrocardiogram, pulse, blood pressure, SpO2), bedside X-ray machine, ambu balloon with mask, breathing kit oxygen, emergency pleural dialysis kit, first aid kit for cardiac arrest,... Patient: Explained about the purpose, procedure to perform the technique, the risks that may be encountered and signed a commitment to practice. presently. After that, the patient does the necessary tests: Measure blood pressure, take pulse, breathing rate, SpO2, weight, height, calculate body mass index,...; Medical records: Fully record the parameters to be monitored and check the results of the tests.
FiO2 100% then gradually reduce to maintain FiO2 > 92% IPAP 8-12 cmH2O EPAP 0-5 cmH2O Support pressure (PS) = IPAP-EPAP The differential pressure between IPAP and EPAP should maintain about 5cmH2O, BiPAP usually starts IPAP/EPAP at 8/3 or 10/5 cmH2O. + Set alarm limit levels
Set alarm limits, set levels depending on the specific medical condition of each Patient.
+ Carry out mechanical ventilation for the patient
Explain to the patient to understand and cooperate, then place the nose or nose mask on the patient, the operator's hand holds the mask so that it fits tightly, check the instructions If the patient is on a ventilator, when the patient is on the ventilator, cooperate well, then use a fixed wire
+ Adjust ventilator parameters:
If PaO2 decreases
Increase FiO2 every 10% to reach SpO2 > 92%. Increase IPAP and EPAP 2cmH2O each time, can increase IPAP to 20cmH20 and EPAP increase to 10-12cmH2O. If PaO2 increases: Reduce FiO2 every 10% to reach SpO2 > 92%
In case PaCO2 increases (pH < 7.3): Increase IPAP and EPAP by 2cmH2O each time, can increase IPAP to 20cmH20 and EPAP increase to 10-12cmH2O.
In case PaCO2 decreases (pH>7.45): Reduce IPAP and EPAP by 2cmH2O each time.
3.3 Monitor Ventilator Performance, airway pressures and alarm status; Monitor anti-machine status: See if the patient is cooperative, if not, need to guide and motivate the patient. In case of failure, the patient's blood oxygenation does not improve, then invasive mechanical ventilation can be intubated; Blood pressure, pulse, ECG, SpO2, regular patient consciousness; Periodic blood gas testing every 12-24 hours depending on the condition of the disease, emergency when there are abnormal developments; Periodic chest X-ray every 1-2 days, emergency scan when there are abnormal developments.

Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
SEE MORE2 commonly used methods of artificial ventilation Artificial ventilation (machine ventilation): What you need to know Surfactant pump for neonatal respiratory failure: Things to keep in mind