This is an automatically translated article.
The article is expertly consulted by Master, Doctor Nguyen Thi Mai Anh - Doctor of Radiology - Department of Diagnostic Imaging and Nuclear Medicine - Vinmec Times City International General Hospital. Doctor Nguyen Thi Mai Anh has nearly 10 years of experience in the field of diagnostic imaging, especially in imaging breast and thyroid cancer.A subdural hematoma is bleeding in the space around the brain. The subdural hematoma on unenhanced CT scan of the brain revealed the presence and size of the hematoma that formed between the dura mater and the arachnoid.
1. Pathophysiology
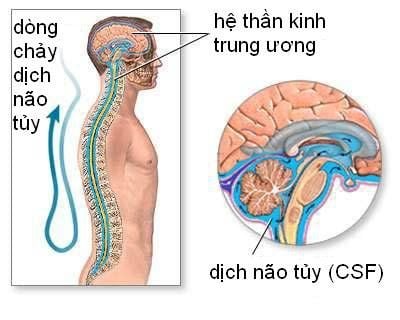
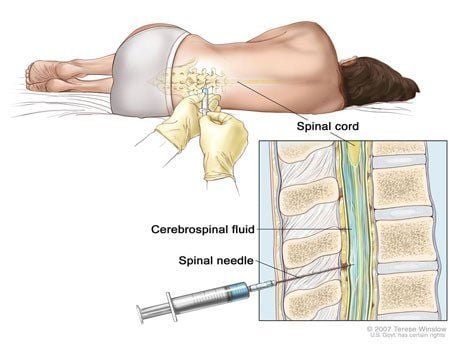
In closed traumatic brain injury, vibrational movements along the diameter of the skull can damage veins, arteries, or brain parenchyma, causing a subdural hematoma. Specifically:The bridging veins that drain blood from the cerebral cortex to the dural sinuses are torn, causing blood to flow into the space between the arachnoid and dura. Usually, increased intracranial pressure or blood clots directly stop venous bleeding. Subdural hematomas due to a laceration of the vein tend to be in the fronto-parietal region. Arterial lacerations can also cause subdural hematomas, which account for about 20-30% of cases, mainly affecting small cortical arteries <1mm in diameter. A subdural hematoma due to an arterial tear tends to be located in the temporal-parietal region. Both arterial and venous causes carry a high risk of death. Another mechanism that causes subdural hematomas is low CSF pressure, also known as decreased intracranial pressure. The cause of this condition is spontaneous or idiopathic CSF leakage, which sometimes also occurs after lumbar puncture. As cerebrospinal fluid pressure decreases, cerebral tension decreases, causing stretching of dependent structures. Dilatation of the glomerulus veins can cause lacerations and ruptures of blood vessels, while a decrease in autologous intracranial pressure leads to cerebral venous stasis. The result is drainage into the subarachnoid space.
2. Symptoms and classification
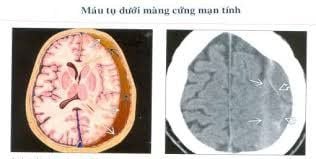
Hình ảnh máu tụ dưới màng cứng mạn tính
Classification of subdural hematoma is determined based on the time from the time of injury, specifically as follows:
Acute: From 1 to 2 days after injury Subacute: From 3 to 14 days after injury Chronic injury: From the 15th day after the injury. This definition is useful only when there is a clear history of trauma or provoking events until the onset of clinical symptoms.
2.1. Acute subdural hematoma Approximately 50% of trauma patients with a subdural hematoma will be comatose immediately after the injury. However, only about 12-38% of these acute patients experience a gradual decline in consciousness afterward. Posterior fossa subdural hematoma often presents with symptoms of increased intracranial pressure, including:
Headache Vomiting Pussy Dilated pupils Mute voice Cranial nerve paralysis Stiff neck Ataxia.

Nếu giảm áp lực tưới máu não có thể dẫn đến nhồi máu não
Apathy Loss of common sense of fear and anger Strange sexual behavior Increased appetite mouth Talk a lot. 2.2. Chronic subdural hematoma may insidious manifestations include:
Headache Light agitation Consciousness disturbance Apathy Lethargy Sometimes convulsions. These symptoms become more pronounced after several weeks of trauma, and may be transient or fluctuating. In chronic subdural hematomas, systemic defects (eg, altered mental status) are more common than focal neurologic findings. Possible focal neurological signs are:
Ipsilateral hemiparesis: Due to the displacement effect of the hematoma, it causes lateral displacement of the brain stem. Hemiplegia on the opposite side: May be the result of a hematoma pressing directly on the cerebral cortex. Chronic bilateral temporal subdural hematomas may present with transient mild paralysis at the extremities and with little pain.
3. Image of subdural hematoma on CT film of the brain

Chụp CT đầu giúp chẩn đoán bệnh
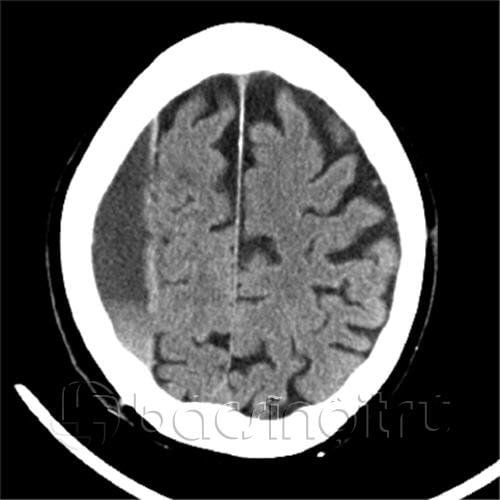
Subdural hematomas can run across joints, but are limited by adhesions of the meninges. So the typical manifestation of this condition is a crescent-shaped lesion.
The subdural hematoma can be clearly observed on acute non-injectable CT cranialography as a crescent-shaped, hyperattenuated mass surrounding the cerebral cortex (Figure 1).

1. Hình ảnh máu tụ dưới màng cứng trên phim CT sọ não không tiêm thuốc hai bên
2. Máu tụ dưới màng cứng mạn tính

3. Hình ảnh máu tụ ngoài màng cứng trên phim CT sọ não không tiêm thuốc
In acute head trauma, imaging of a subdural hematoma on cranial CT plays a key role in both diagnosing the lesion and determining appropriate initial treatments. In addition, any head injury may be present with a subdural hematoma, the clinical manifestations of which are difficult to distinguish. Therefore, determining the natural progression of each lesion is important, helping to have a specific treatment.
Vinmec International General Hospital is a high-quality medical facility in Vietnam with a team of highly qualified medical professionals, well-trained, domestic and foreign, and experienced.
A system of modern and advanced medical equipment, possessing many of the best machines in the world, helping to detect many difficult and dangerous diseases in a short time, supporting the diagnosis and treatment of doctors the most effective. The hospital space is designed according to 5-star hotel standards, giving patients comfort, friendliness and peace of mind.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Recommended video: