This is an automatically translated article.
The article was professionally consulted by Specialist Doctor II Cao Thi Thanh - Pediatrician - Pediatrics - Neonatology Department - Vinmec Hai Phong International General HospitalNot only occurs in adults, infants and children are also at risk of hypoglycemia. This condition can cause dangerous complications affecting the health of the child, and can even cause brain damage if not diagnosed and treated promptly. Let's learn more about this issue through the article below.
1. What is neonatal hypoglycemia?
Hypoglycaemia is common in neonates and may be transient in the early postpartum period. However, persistent hypoglycemia can cause brain damage and long-term consequences for the child.
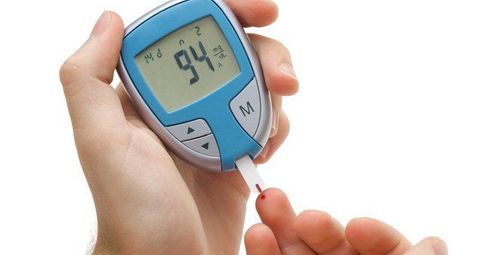
According to the American Academy of Pediatrics, neonatal hypoglycemia is defined when the child's blood glucose level is <2.6mmol/l.
2. Why do babies have low blood sugar?
There are many causes of hypoglycemia in infants such as:2.1 Hypoglycaemia due to increased insulin Due to changes in the mother's metabolism: Diabetes, water or medication infusion during pregnancy.
Congenital factors: The state of mutations in genes encoding the regulation of insulin secretion by pancreatic Beta cells such as genes Kir6.2, KCNJ11, ABCC8, SUR1,...
Secondary hyperinsulinemia: Children Asphyxiation, the mother during treatment with terbutaline, contracted Beckwith-Wiedemann syndrome. Besides, increasing insulin must also mention some causes as follows:
Sudden stop of high glucose level; The umbilical artery catheter is in the wrong position; Exchange transfusion with high blood glucose concentration; Tumors produce insulin, increase Beta cells. 2.2 Children larger for gestational age Besides the cause of maternal diabetes, there are cases where the cause cannot be confirmed. This is a high-risk group, so the mother should be screened for blood sugar.
2.3 Decreased Glucose Production or Storage Usually occurs in the following situations:
Premature babies; Intrauterine growth retardation; Diet with insufficient energy; Feeding children late; 2.4 Increased use/decreased production of Glucose Stress at birth: Infants with sepsis, shock, hypothermia, respiratory failure, post-resuscitation period. Congenital metabolic disorder. Endocrine disorders. Polycythemia. The mother is taking beta blockers.

3. Signs of hypoglycemia in babies
In newborns, symptoms of hypoglycemia usually appear from 3 to 48 hours after birth, including the following signs:
Rapid drop in body temperature, pale skin, cyanosis, cold hands and feet; Gastrointestinal symptoms such as abdominal pain, vomiting, irritability; Rapid, rapid, forceful breathing; In severe cases, convulsions and coma may occur. 41% of cases of neonatal hypoglycemia usually occur in premature, low birth weight infants less than 2.5 kg. According to experts, the disease can have a serious impact on the child's nerves later in life. Therefore, infants need to be diagnosed and treated promptly.
4. Treatment of hypoglycemia in infants

4.2. Adjust blood sugar The goal of maintaining serum glucose ≥ 2.6 mmol/L in the first day postpartum and ≥ 2.8 mmol/L in the following days.
Adjustment of blood glucose is made step by step according to the degree of hypoglycemia, with or without symptoms as follows:
4.2.1 Dietary Adjustment Applies to serum Glucose level of 2 – 2.6 mmol /L and no symptoms. Breastfeeding soon after birth. In some cases, infants are at risk for early feeding within the first hour of life and blood glucose screening 30 minutes later. If the child cannot breastfeed, express milk and feed the child with an alternative method, the amount of food is enough according to the needs of the day. Meals can be increased to 12 meals/day. Monitor blood sugar before eating. 4.2.2 Infusion Indicated for hypoglycemia
Children with symptoms. Blood glucose <1.4 mmol/L Blood glucose <2.2 mmol/L (40mg/dL) when adjusted by diet. Children cannot eat. With a glucose level <1.4 mmol/L, 10% glucose solution should be administered intravenously, 2ml/kg over 1 minute, then intravenous fluids.
The rate of infusion (GIR) ranges from 6 to 8 mg/kg/min, infusion of 10% glucose solution with a maintenance dose of 80-120 ml/kg/day. Peripheral intravenous infusion of 10% and 12% glucose concentrations is recommended. (<12%)
Infusion rate: for 10% Glucose solution it is 0.6 x weight x GIR and 12% Glucose solution is 0.5 x weight x GIR.
Monitor blood sugar every 3 hours until blood glucose is > 2.6 mmol/L in 2 consecutive tests.
If glucose is low, gradually increase fluid volume or glucose concentration. Fluids with glucose concentration less than 12.5% allow peripheral intravenous infusion, fluids with Glucose concentration above 12.5% require central intravenous infusion
4.2.3 Persistent hypoglycemia If persisting for more than 2 days At an infusion rate of up to 12 mg/kg/min, treatment with diazoxide or hydrocortisone may be necessary and the cause must be found to treat (Test insulin and blood cortisol before Glucocorticoid therapy). Hydrocortisone dose 5 mg/kg/day, divided into 2 doses, intravenous or oral. The use of Diazoxide or Glucagon requires consultation with an endocrinologist. 4.2.4 Monitor when blood glucose is normal If serum glucose is stable with intravenous therapy:
Start feeding 20ml/Kg/day Gradually increase feed intake and gradually decrease fluid intake until complete feeding is achieved. Check blood glucose after each change of treatment, pay attention to check blood glucose before eating.
4.3. Treatment according to the cause In case of persistent hypoglycaemia with the need for an infusion rate of more than 8 mg/kg/min for more than 1 week, consultation with an endocrinologist is required for appropriate treatment. Hypoglycemia due to a number of uncommon causes.
Hypoglycemia in infants is a dangerous disease, so when seeing a child with unusual symptoms, parents need to immediately take the child to medical facilities for advice by doctors. timely diagnosis and treatment.
As a key area of Vinmec Health system, Pediatrics Department always brings satisfaction to customers and is highly appreciated by industry experts with:
Gathering a team of top doctors and nurses in Pediatrics : consists of leading experts with high professional qualifications (professors, associate professors, doctorates, masters), experienced, worked at major hospitals such as Bach Mai, 108.. Doctors All doctors are well-trained, professional, conscientious, knowledgeable about young psychology. Besides domestic specialists, the Department of Pediatrics also has the participation of foreign experts (Japan, Singapore, Australia, USA) who are always pioneers in applying the latest and most effective treatment regimens. Comprehensive services: In the field of Pediatrics, Vinmec provides a series of continuous medical examination and treatment services from Newborn to Pediatric and Vaccine,... according to international standards to help parents take care of their baby's health from birth to childhood. from birth to adulthood Specialized techniques: Vinmec has successfully deployed many specialized techniques to make the treatment of difficult diseases in Pediatrics more effective: neurosurgery - skull surgery, stem cell transplantation. blood in cancer treatment. Professional care: In addition to understanding children's psychology, Vinmec also pays special attention to the children's play space, helping them to have fun and get used to the hospital's environment, cooperate in treatment, improve the efficiency of medical treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.