This is an automatically translated article.
According to many studies, all classes of antihypertensive drugs combined with diuretics increase the effectiveness of lowering blood pressure. The selection of commonly used antihypertensive drugs for combination therapy should also be carefully considered.
1. Why combine antihypertensive drugs?
According to medical studies, patients need to take combined oral antihypertensive drugs because:
Hypertension is a multi-system disease, it is necessary to combine many different drugs to help control blood pressure more closely ; Combination of drugs to reduce unwanted effects, and at the same time increase the effectiveness of lowering blood pressure; Combining 2 commonly used antihypertensive drugs is easier to achieve the treatment goal than using only 1 (if the dose is doubled, it will be less effective). In addition, the combination of antihypertensive drugs also plays a role in diabetes. Good blood pressure control is key in protecting the heart and kidneys in diabetics. Most patients require a combination of drugs to achieve recommended blood pressure goals, and many patients require ≥ 3 drugs. Thiazide/thiazide-like diuretics combined with antihypertensive drugs are common.

Bác sĩ là người chỉ định phối hợp thuốc hạ huyết áp
2. When should combination oral antihypertensive drugs be used?
2.1. Hypertension grade II and III According to the recommendations of the Vietnam Hypertension Sub-Association in 2015, it is necessary to use combination oral antihypertensive drugs when:
Blood pressure ≥ 160/100 mmHg; Systolic blood pressure > 20 mmHg or diastolic blood pressure > 10 mmHg above target blood pressure. In particular, when taking a commonly used antihypertensive drug but not reaching the target after 1 month, the combination of ACE inhibitor/alpha receptor blocker and Calcium channel blocker or blood pressure drug combined with thiazide diuretic is preferred.
2.2. Grade I hypertension with cardiovascular risk In combination with antihypertensive drugs when stratification of cardiovascular risk is moderate/high/very high:
Having 3 or more CVD risk factors; Target organ damage; Symptomatic cardiovascular disease; Diabetes; Chronic kidney disease stage 3 or 4.

Người bệnh có bệnh lý đái tháo đường
3. Some commonly used antihypertensive drugs
3.1. Diuretics Diuretics are chosen as first-line agents for hypertension because they reduce morbidity and mortality. It is recommended to use low-dose diuretics in combination with antihypertensive drugs. The different groups of diuretics include:
Thiazide/thiazide-like diuretics: The mechanism of renal tubular sodium excretion and reabsorption contributes to hypotensive and hypovolemic effects. Concomitant use with non-steroidal anti-inflammatory drugs should be avoided, or in patients with a history of gout, and taking lithium due to the high risk of toxicity; Potassium-sparing diuretics: There are two main roles in the treatment of hypertension. One is that it can be combined with a thiazide/thiazide-like diuretic to limit potassium loss. The second is a blocker of sodium/potassium ion exchange in the distal tubule, which plays an important role in lowering blood pressure in treatment-resistant patients due to hyperaldosteronism; Loop diuretics: No significant role in hypertension except in renal and/or cardiac failure.

Sử dụng thuốc hạ huyết áp theo đúng chỉ định của bác sĩ
3.2. Calcium channel blockers are a group of drugs commonly used in angina and hypertension. There are two main groups:
Dihydropyridines have a more selective blocking effect on calcium L channels in vascular smooth muscle, causing vasodilation that reduces vascular resistance and blood pressure. Using slow-acting dihydropyridine is safer and has fewer dangerous side effects. Non-dihydropyridine group with therapeutic doses will block calcium channels in myocardial cells, thereby reducing cardiac output. Extreme caution must be exercised when co-administering beta-blockers. 3.3. The mechanism of action is to bind the zinc ion (Zn) of the ACE inhibitor to the radicals of the ACE inhibitor, preventing the conversion of angiotensin I to angiotensin II. As a result, angiotensin II decreases, leading to vasodilation and hypotension. Angiotensin II also causes harmful effects on the cardiovascular system and changes the structure of the heart, blood vessels and kidneys in hypertension and other cardiovascular diseases.
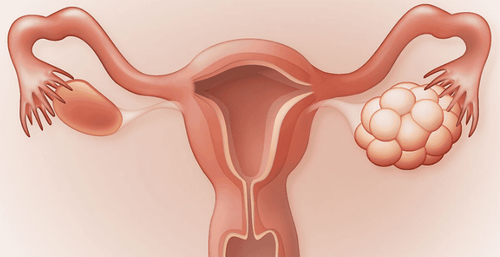
Avoid taking the drug in pregnant women due to the risk of fetal kidney development abnormality. The drug should not be used in patients with bilateral renal artery stenosis to avoid worsening renal failure.

Một số đối tượng không nên sử dụng thuốc ức chế men chuyển
3.4. Angiotensin receptor blockers These drugs block angiotensin II type 1 receptors, leading to vasodilation and hypotension, with effects similar to those of ACE inhibitors. The drug causes a decrease in peripheral resistance, little change in heart rate and cardiac output... Compared with ACE inhibitors, the drug does not have the effect of increasing Bradykinin and does not cause cough like ACE inhibitors. The drug is generally well tolerated in patients unable to take other medications. Caution and contraindications as ACE inhibitors.
4. How to use combination antihypertensive drugs
4.1. Combination of 2 drugs Angiotensin-converting enzyme inhibitors (ACEIs)/Angiotensin II receptor antagonists (ARBs) + Calcium channel blockers (CCBs) Low-dose ACE inhibitors and calcium antagonists (except Dihydropyridines) have been shown to lower pressure and protein reduction is more effective than using them alone. Combining an ACE inhibitor with dihydropyridine can reduce the side effect of ankle edema.
Angiotensin-converting enzyme inhibitors/Angiotensin II receptor antagonists + Thiazide diuretics/thiazide analogues; Calcium channel blockers + Thiazide/thiazide-like diuretics: There is an advantage in primary stroke reduction given other combinations; 4.2. Combination of 3 drugs When having to use the 3rd and 4th drug combinations, it must also be based on the principle of choosing drugs with different mechanisms of action. Common beneficial combinations are:
Angiotensin-converting enzyme inhibitors or Angiotensin II receptor antagonists; Calcium channel blockers; Thiazide diuretics / Thiazide analogues.

Phối hợp 3 thuốc hạ huyết áp phối hợp
4.3. Combination of drugs in 1 tablet It is recommended to use combination tablets not only to reduce the amount of medication taken, but also have the following benefits:
Efficacy: Converting the separate combination to a fixed dose of the same strength can reduce blood pressure an additional 15.6/7.7 mmHg after 1 month of treatment, and a further reduction of 23.3/11.3 mmHg after 3 months. The survival rate of patients receiving a single dose is also about 10% higher; Increase treatment adherence: Switching from a separate combination to a combination of 1 tablet/day helps patients more easily adhere to treatment; Economic savings: Fixed dose combination helps to save costs for the national health fund as well as for the patients themselves. Note, most elderly people need more than one antihypertensive drug to control blood pressure, so the combination of drugs should be recommended by the doctor. The wrong combination of drugs is one of the causes of resistant hypertension.
In general, the combination of drugs in the treatment of hypertension is a matter of concern. According to medical guidelines, most cases require a combination of two commonly used antihypertensive drugs, while the use of combined oral antihypertensive drugs must rely on separate mechanisms. Studies also show that a fixed-dose combination in one pill is more beneficial.
Reference source: aafp.org