This is an automatically translated article.
The article was professionally consulted by Dr. Nguyen Van Dinh - Head of Respiratory - Asthma - Allergy - Clinical Immunology Unit, Vinmec Times City International Hospital.Asthma (asthma) is a chronic inflammation of the airways, leading to intermittent shortness of breath due to spasm of the bronchi. Pregnant women with bronchial asthma will be very dangerous because it can cause lack of oxygen to the fetus.
1. Effects of bronchial asthma in pregnancy and fetus
Most asthmatics can have normal pregnancies and births like healthy people. However, severe cases of asthma, which is not well controlled, can have negative effects on the fetus due to prolonged hypoxia. Many studies in the past 20 years have shown that cases of bronchial asthma in pregnant women are at risk of premature delivery, low birth weight or certain diseases (tachycardia, convulsions, hypoglycemia, etc.). .) are higher than those of mothers without the disease. However, this risk is very small if asthma in pregnant women is stabilized and it can be minimized by maintaining optimal asthma control throughout pregnancy.
2. Management of bronchial asthma before pregnancy
These recommendations apply to any woman who is pregnant:
All women need to get at least 400 mg of extra folic acid. Using folic acid may reduce the risk of neural tube defects. Folic acid should be started before pregnancy and continued until at least the end of the first trimester. Stop smoking and drinking alcohol, do not use stimulants. Coffee drinking should be limited to less than 250 mg per day while trying to conceive and during pregnancy. Blood tests for measles, chickenpox, HIV, and hepatitis B may be recommended before becoming pregnant. For women with bronchial asthma who want to become pregnant, it is necessary to be examined and consulted by a doctor to ensure that their asthma is under stable control before becoming pregnant.

3. Management of bronchial asthma in pregnancy
During pregnancy, care of pregnant women with bronchial asthma requires the involvement of an asthma specialist and an obstetrician. Asthma specialist visits are ordered based on severity of asthma during pregnancy. Most women need to see an obstetrician every two to four weeks until 28 weeks of pregnancy. Between weeks 28 and 36, most pregnant women with asthma need to see their doctor every two weeks. Pregnant women with bronchial asthma usually visit a doctor once a week between 36 weeks and delivery.
Many pregnant women, when their condition is stable or fear the drug's risk to the fetus, stop taking the drug on their own, which can trigger a severe asthma attack that threatens both mother and baby. Therefore, do not arbitrarily stop the drug during pregnancy. Do not arbitrarily take other drugs without consulting a doctor because it can aggravate asthma or affect the fetus.
3.1. Monitoring Maternal Lung Function
Normal lung function is important for the health of the mother and the well-being of the baby. Lung function can be monitored in the hospital. Home monitoring often provides important information when asthma symptoms worsen, especially during the night or upon waking.
Pregnant women can have their lung function monitored at home with a peak flow meter to measure peak expiratory flow. Depending on the frequency of attacks, your doctor may recommend measuring twice daily: once upon waking and again 12 hours later. A decrease in peak expiratory flow signals worsening of asthma and requires emergency treatment, even if the patient feels well.
Pulmonary function testing performed in the clinic is also beneficial to distinguish shortness of breath associated with worsening asthma from the shortness of breath that many women experience during pregnancy.
Your baby's well-being:
Your baby's well-being is carefully monitored during visits throughout pregnancy. These visits are especially important for women with asthma.
In addition, women who are more than 24 weeks pregnant need to have their baby's movements monitored. If your baby is not moving normally, see an obstetrician immediately. This is especially true for pregnant women who have asthma or have an asthma attack.
3.2. Avoiding asthma triggers Many simple steps can help control the environmental factors that worsen asthma in pregnant women. These steps include:
Avoiding exposure to specific allergens to which the patient has pre-existing allergies to pet dander, house dust, and nonspecific irritants, such as tobacco smoke, odors and pollen. If the pregnant woman is allergic to house bugs or house dust, keep the living environment clean, change the sheets and pillows weekly, limit carpets and fabric furniture in the house, can use pillows and blankets with membranes. house mite prevention. Avoid active and passive smoking (inhaling secondhand smoke from loved ones or people around you who smoke) Women who will become pregnant with bronchial asthma during flu season need a flu shot. There is no risk from influenza vaccination on fetal development. 3.3. Education Understanding asthma helps patients better manage their symptoms, prevent asthma attacks, and respond to asthma attacks. Asthma education helps patients develop strategies to recognize the signs and symptoms of asthma, avoid triggers that can trigger an asthma attack, and use asthma control medications consistently. right way. From there, it is necessary to develop an individualized treatment plan for sudden attacks.
3.4. Drug treatment

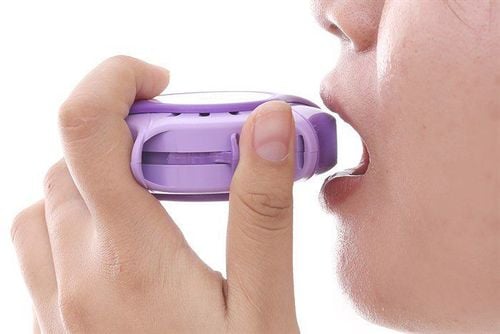
In rare cases, the drugs used to treat asthma in pregnancy are the same as those used to treat common asthma. The type and dose of asthma medications will depend on many factors. In general, inhalers are recommended because of the few adverse effects on the mother and the baby. Drug type or dose adjustment during pregnancy may be necessary to avoid changes in maternal metabolism and changes in asthma severity.
Safety of asthma control drugs: It is difficult to prove that asthma control drugs are completely safe during pregnancy. However, asthma medications have been used by pregnant women with asthma for many years, demonstrating that most of them almost certainly pose little or no risk to the mother or child. child.
It is important to weigh the risks of asthma control medications compared with the severe harms of untreated asthma.
Asthma attacks in pregnant women can reduce the oxygen supply to the baby, leading to fetal growth retardation or fetal distress. Indeed, it is important to use asthma medication in pregnant women to prevent asthma symptoms. In the majority of cases, untreated asthma poses a greater risk to both mother and child than the use of asthma control medications.
If you have unusual symptoms, you should be examined and consulted with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.