This is an automatically translated article.
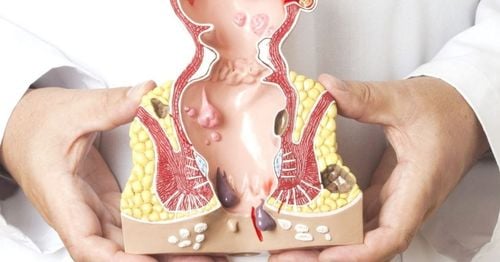
The article is professionally consulted by the Doctor of General Surgery.If not treated early, hemorrhoids can cause unpredictable consequences, significantly affecting the patient's health, daily life as well as work. Vinmec Hospital doctors will provide information on effective treatments for this unpleasant disease.
Note the principles of hemorrhoid treatment:
Do not treat symptomatic hemorrhoids, unless there are complications. Only treat hemorrhoids when there are disorders affecting life, work and health. Depending on the specific injury of hemorrhoids, choose the appropriate treatment method.
1. Medical treatment
Medical treatment is applied to grade I hemorrhoids and mostly grade II hemorrhoids.Diet high in fiber (vegetables, flour, whole grains) and stool softeners, drink extra water. Avoid straining when passing stool to help limit the prolapse of hemorrhoids. Soak the anus in warm water 2-3 times a day, 10 minutes each time. Use rectal drugs, drugs that strengthen the vascular wall. Don't assume that anorectal bleeding is always caused by hemorrhoids. Cancer must be ruled out by colonoscopy and colonoscopy.
2. Surgical treatment
2.1. Surgical interventions
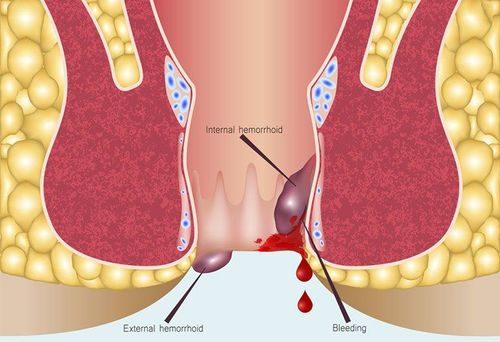
Elastic band ligation is the best method for grade I and II internal hemorrhoids (not for external hemorrhoids). Your doctor will warn you in advance that when hemorrhoids fall off, from day 6 to day 10 there may be light bleeding. If you have pain, urinary retention, and fever, a follow-up visit is needed to rule out an infectious syndrome of the perineum. Sclerotherapy is indicated for grade I and grade II hemorrhoids, especially in immunocompromised patients or with coagulopathy. Sclerotherapy is performed by injecting 1-2 ml of a sclerosing agent, which is 5% phenol, quinine, urea hydrochloride, polidocanol or sodium tetradecyl sulfate, and injected with a needle under the lining of the hemorrhoid. Infrared photocoagulation is indicated for grade I, II hemorrhoids. Hemorrhoid laser ablation is indicated for grade II hemorrhoids. Note: These surgical interventions need to be performed by specialists and should be performed in hospitals.

Các can thiệp thủ thuật cần được thực hiện tại các bác sĩ chuyên khoa và cần được thực hiện tại các bệnh viện.
2.2. Surgical interventions
Direct hemorrhoidectomy according to the methods of Miliant Morgan, Feguson or White heat for grade III and IV internal hemorrhoids, mixed hemorrhoids or complicated hemorrhoids. Direct cutting of hemorrhoids will cause loss of padding. The anal canal should cause the patient to have fecal incontinence. In addition, direct intervention in the hemorrhoids will damage the nerve endings in the anal canal, causing prolonged pain for the patient. In the past 10 - 20 years, doctors have performed surgery that does not directly interfere with the hemorrhoids, but only intervenes above the dentate line and does not aim to remove the hemorrhoids. The principle of these methods is to reduce the blood supply to the hemorrhoid and fix the hemorrhoid back to the anatomical position with tools or sutures.
Longo surgery is indicated for internal hemorrhoids grade II, III and ring hemorrhoids. The principle is to use a loop suture tool to excise a segment of mucosa 2 cm to 5 cm above the dentate line and to place stamens to suture the mucosa. The blood vessels that go to the hemorrhoids are also stitched, which contributes to the shrinking of the hemorrhoids. Advantages: Very little pain (because there are very few sensory receptors above the dentate line), patients can be discharged 1-2 days early after surgery, and soon return to normal activities.
Cons: Difficult to deal with mixed hemorrhoids with too much rectal mucosal prolapse; The price of a dedicated press connection machine is still high.
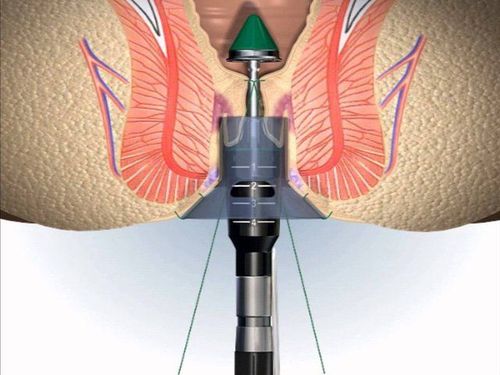
Phẫu thuật Longo rất ít đau bệnh nhân có thể ra viện sớm 1-2 ngày sau mổ, và sớm trở lại với sinh hoạt bình thường
3. Note when treating hemorrhoids
Hemorrhoids need to be examined early with an anorectal specialist. Depending on the extent of damage to the hemorrhoid, there is an appropriate treatment. Complications of acute hemorrhoids can include pain, infection, bleeding, and urinary retention. The longer hemorrhoids go untreated, the harder it is to control late complications. Should not be shy because self-esteem is a disease in the private area should be shy to go to the doctor.3.1. What should you eat when you have hemorrhoids?
Hemorrhoids are very common, but each of us can prevent ourselves by having healthy eating and living habits: Drink more water, defecate on time, avoid sitting for a long time, should not abuse alcohol and hot spicy foods. ,... This also applies to reducing hemorrhoid symptoms, supporting disease treatment.3.2. Eat plenty of foods that contain fiber
Recommended foods include: Whole grains (barley, wheat, corn, brown rice, millet, rye, oats, ...), fruits, vegetables, ... help increase stool volume, stool softness.
3.3. Drink a lot of water
Drink 2 liters of water per day with other liquids, except alcohol, to aid digestion and soften stools.3.4. Hemorrhoids eat fruit, what fruit is suitable?
Everyone should eat the recommended amount of fiber daily, which is 25g per day for women and 40g per day for men. Adding more fruits such as bananas, papaya, grapefruit, ... will help improve symptoms, reduce bleeding hemorrhoids effectively.
Sản phẩm bổ sung chất xơ.
You can use dietary fiber supplements to help soften stools and go to the toilet more regularly every day.
3.5. Try to go to the toilet regularly & don't push too hard when going to the toilet
It is necessary to make a habit of going to the toilet, you should defecate as soon as you feel sick, because fasting causes stools to stay for a long time in the rectum and anus, the rectum will gradually absorb water in the stool, causing stools. dry, stagnant and harder to walk.
The more you push harder when going to the toilet, the more pressure you put on the veins in the lower rectum, the easier it is for the hemorrhoids to bleed and swell. It is necessary to avoid reading newspapers, watching mobile phones when having a bowel movement
Daily exercise is necessary to promote health, prevent constipation and reduce pressure on veins, especially those who have to regularly stand or sit for a long time
3.6. Limit sitting for too long
Sitting for too long, especially on the toilet will put a lot of pressure on the veins in the anus, making hemorrhoids worse. If due to the nature of work, try to regularly exercise, both to limit hemorrhoids and good for the spine.
Symptoms of hemorrhoids are not too difficult to recognize. But most are subjectively ignored by patients or subjectively thinking that they can treat themselves at home. The specific symptoms of anal bleeding outside of hemorrhoids can be from many other dangerous diseases to watch out for such as colorectal polyps, anal canal cancer, colorectal cancer,... When having problems Regarding hemorrhoids, you can contact Vinmec International General Hospital for support from experienced doctors in this field.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.