This is an automatically translated article.
Most patients with uterine adhesions syndrome will present with less menstrual bleeding (oligomenorrhea) or no amenorrhea (amenorrhea) and affect reproductive function. So this situation makes many women worry whether they can cure uterine adhesions and can get pregnant?
1. What is uterine adhesions?
Adhesions of the uterus is an acquired syndrome characterized by partial or complete fusion of the anterior and posterior wall of the uterus. Based on the degree, uterine adhesions are usually classified into two types as follows:
Uterus fully adherent: the anterior and posterior uterine walls are completely fused and in this case, women are likely to have ectopic pregnancy. amenorrhea or secondary infertility. Partial or scattered uterine adhesions: the degree of adhesion is not complete, and women may have fewer menstrual days and less menstrual bleeding. However, women can still get pregnant but will have uterine adhesions during pregnancy. Some causes of uterine adhesions include:
Injury to the uterus through surgical curettage or cleaning of the uterine wall after a miscarriage, abortion, or treatment of certain medical conditions in the uterus such as heavy bleeding. In particular, abortion is one of the highest risk factors for uterine adhesions syndrome because curettage of the uterine lining can cause scar tissue to stick. Other types of uterine surgery such as removal of fibroids, polyps, or uterine correction surgery that can cause scar tissue formation are also risk factors for uterine adhesions. Factors that cause inflammation of the uterus known as endometriosis and sporadic metritis have been associated with uterine adhesions syndrome. Bacterial infection and inflammation of the uterus (genital tuberculosis) and parasites such as blood flukes are also risk factors for uterine adhesions.
2. How to diagnose uterine adhesions?
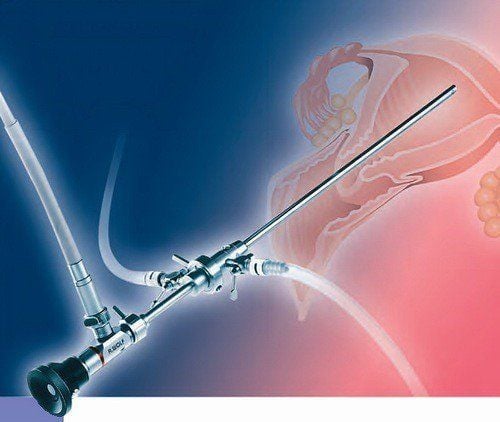
Routine gynecological examination almost does not detect uterine adhesion syndrome. The gold standard in the diagnosis of uterine adhesions is endoscopic imaging. Some tests in the diagnosis of uterine adhesions include:
Hysterosonogram X-ray of the uterus and fallopian tubes (Hysterosalpingogram (HSG) Transvaginal ultrasonography of the uterus, Blood tests to detect it. tuberculosis or schistosomiasis.

Siêu âm đầu dò giúp bác sĩ chẩn đoán và điều trị dính buồng tử cung
3. Treatment of uterine adhesions
Can uterine adhesions be cured is a question that women always wonder about. Treatments for uterine adhesions focus on restoring the uterus to its original size and shape. Thereby, helping to relieve pain, regenerate the menstrual cycle and improve the chances of conception. Therapies can be divided into three main approaches: treatment - laparoscopic surgery, prevention of re-adhesion and uterine restorative therapies. Specifically, the treatment options for uterine adhesions include:
3.1. Laparoscopic surgery This is the most common treatment for uterine adhesions.
In addition to diagnostics, hysteroscopy is used to cure adhesions by cutting the adhesions with very fine scissors, lasers, or other instruments that use hooks or electrodes. The hysteroscope allows the doctor to magnify and directly view the uterus for precise resection of uterine adhesions. The purpose of surgery for uterine adhesions is to remove scar tissue and restore the shape of the uterine cavity.
3.2. Prevention of Re-adhesion Several procedures have been developed to prevent re-adhesion of the uterine wall after laparoscopic surgery because scar tissue may re-adhesive including:
Foley catheter: this is one of the devices. was first developed to separate the uterine walls to prevent recurrent adhesions. A Foley catheter may be inserted into the uterus for 5 to 7 days along with a bag to remove fluid from the uterus. Another method of curing uterine adhesions to prevent re-adhesion is a balloon stent made of silicone and shaped to fill the uterine cavity. Finally, the application of certain chemicals such as hyaluronic acid has been shown to help prevent re-adhesion of the uterus. Although the mechanism is not completely understood, it is believed that hyaluronic acid acts as a temporary barrier to prevent re-adhesion and may also promote tissue repair. 3.3. Uterine Restoration Therapy Hormone therapy such as estrogen supplementation has been suggested to help promote tissue repair and repair of the lining of the uterus. Therefore, oral contraceptives, patches, or other medications containing estrogen may be prescribed prior to surgery to prevent scar tissue formation and promote endometrial healing.
In addition, after the procedure, the doctor may prescribe hormones to return the lining of the uterus to normal to help women have normal periods again.
Antibiotics are also often prescribed after a hysterectomy. Although antibiotics do not directly treat uterine adhesions, they help prevent infection and inflammation that can damage the uterus and trigger re-adhesion of the uterine wall.

Liệu pháp hormone được ứng dụng trong chữa dính buồng tử cung
3.4. Stem cell therapy Clinical trials of stem cell therapy are underway to determine whether it can regenerate the uterine wall, especially in subjects with severe uterine adhesions.
Stem cells are undifferentiated cells (stem cells) that can be programmed to develop into almost any cell in the body, including the stromal cells in the uterus. Stem cell therapies mainly focus on regenerating the endometrium that has been damaged by adhesions and surgery. Initial clinical trials have demonstrated that stem cell therapy is safe and possibly effective in helping to regenerate the uterine wall as well as helping to return menses and improve fertility. Clinical trials of root therapy for uterine adhesions are currently underway.
Thus, although uterine adhesion syndrome is a disorder of the menstrual cycle and affects reproductive function. However, uterine adhesion syndrome can be treated with different methods, helping women who are infertile due to uterine adhesion syndrome can have children after treatment.
In order to help customers detect and treat other gynecological diseases early, Vinmec International Hospital has a basic gynecological examination and screening package, helping customers detect early inflammatory diseases Easy, inexpensive treatment. Basic gynecological examination and screening package for female customers, has no age limit and may have the following symptoms:
Pain, itching in the vagina Female customers have several risk factors such as poor personal hygiene, unsafe sex, abortion, ... Female customers have other symptoms such as: Abnormal vaginal discharge, itching, pain in the intimate area, abnormal vaginal bleeding . Irregular bleeding in the vaginal area Menstrual problems: irregular periods, irregular periods Irregular vaginal discharge (with a foul odor, a different color) If you have unusual symptoms, you should be examined and consulted with a specialist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.