This is an automatically translated article.
Tularemia or tularemia is an acute bacterial infection caused by a bacterium called Francisella Tularensis. This is a rare disease that is transmitted directly from a variety of mammals to humans or by insect bites. Symptoms such as headache, abdominal pain, diarrhea and nausea are the sudden onset of the disease. All of these symptoms are accompanied by a fever, which can be as high as 40 °C (104 °F).1. How is Tularemia diagnosed?
Diagnosis of Tularemia is difficult because it is a rare condition and its symptoms can be confused with more common conditions. Usually, depending on how the bacteria enter the patient's body, it will lead to different symptoms of Tularemia, specifically:
Infection through the sting: at the wound site, where the bacteria enter will develop red papules and quickly develop into ulcers, causing the lymph nodes to swell, causing pain and possibly festering. Infection through the digestive tract: if the patient ingests the pathogenic Francisella Tularensis bacteria, symptoms of sore throat, abdominal pain, diarrhea and vomiting will appear. Infection through the respiratory tract: bacteria through the respiratory tract enter the patient's body causing cough, chest pain and difficulty breathing. If the patient discovers that he or she has the above symptoms, it is necessary to see a specialist doctor to examine and perform blood tests and other tests to help confirm the diagnosis.
2. Essential points in the diagnosis of Tularemia
To be able to initially make a diagnosis of Tularemia, doctors will base on the following essential points:
The patient presents with fever, headache, nausea and severe fatigue; Entrance papules progress to ulcers; The lymph nodes in the affected area are gradually enlarged; The patient has a history of exposure to rabbits or other rodents or bites from arthropods (mites, summer mites); Culture of ulcer fluid, blood or lymph node aspirate will show bacteria, or a positive serological reaction. Tularemia has been evaluated as a disease of wild rodents, especially rabbits and water rats. Francisella (Pasteurella) Tularensis is the main bacterium that causes disease in humans as well as in some animal species.
Most of the sick people often come into contact with animal tissues such as skinning rabbits or trapping water rats, or eating infected animals. In humans, the infection will often be local and sometimes widespread, but almost completely without symptoms. The incubation period for Tularemia is 2 to 10 days.

Bệnh Tularemia được đánh giá là bệnh của các loài gặm nhấm hoang dã, đặc biệt là ở thỏ và chuột nước
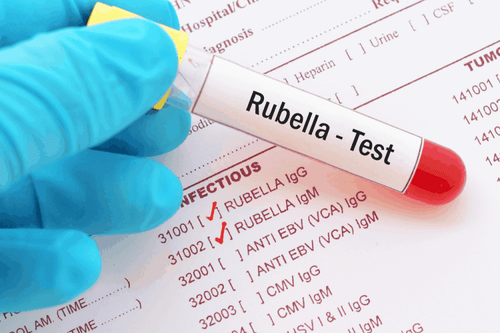
2.1. Subclinical manifestations Doctors will use serology to diagnose Tularemia, because to culture bacteria from blood, a special medium is required. In addition, the disease is highly contagious to laboratory workers during manual handling of infected specimens. During the second week or so, a titration > 1:80 in the agglutination reaction is positive.
2.2. Differential Diagnosis Since the symptoms of the disease can be confused with more common conditions, the differential diagnosis should be made from other fungal or bacterial diseases, rickettsial and meningococcal diseases, and meningococcal disease. infectious mononucleosis, cat scratch disease.
During the course of the disease, differential diagnosis of Tularemia will be made with influenza, typhoid and typhus, pneumonia. After that, will continue to be differential diagnosis with plague, anthrax, nonspecific lymphadenitis, necrotizing tonsillitis, sepsis, malaria, diphtheria, tuberculosis, mumps, brucellosis, limboretikulozom benign, infectious mononucleosis.
2.3. Complications of Tularemia Tularemia causes fever, inflammation of the lymph nodes, and damage to many other organs such as the eyes, lungs, and digestive tract. Patients with Tularemia may experience complications such as meningitis, pericarditis, perisplenic inflammation, pneumonia, osteomyelitis caused by Francisella Tularensis bacteria through the blood.
3. Treatment of Tularemia
Patients with suspected Tularemia will be admitted to hospital for clinical reasons, the room should be covered with mesh at the windows to prevent transmission. Streptomycin, Gentamycin, 3rd generation Cephalosporins and Rifampicin are antibiotics that are effective in the treatment of Tularemia.
3.1. Treatment with antibiotics The preferred antibiotic is Streptomycin (use more Chloramphenicol if accompanied by meningitis):
Streptomycin: For adults, 1g of Streptomycin will be injected intramuscularly every 12 hours, and for children children would be 15mg/kg IM every 12 hours for a continuous period of 7 to 10 days (for moderate to severe disease). Chloramphenicol: If the patient has signs of meningitis, 12.5 to 25 mg/kg IV chloramphenicol or doxycycline 100 mg twice daily should be administered every 6 hours for 14 to 21 days. 3.2. Other Alternatives Alternatives to Streptomycin include:
Chloramphenicol: 12.5 to 25 mg/kg IV every 6 hours (for meningitis only because there are many alternatives available) more effective and safe); Ciprofloxacin: For mild disease, give the patient 500 mg orally every 12 hours; Doxycycline: For mild disease, give the patient 100 mg orally every 12 hours; Gentamicin: Every 8 hours, administer 1 to 2 mg/kg IM or IV every 8 hours (for moderate to severe disease). In cases where the patient cannot use the intravenous line, oral doxycycline or ciprofloxacin should be substituted (in both adults and children). However, recurrence is possible with all of these drugs, and they do not prevent lymph node festering.
Continuous saline dressings are beneficial for major skin lesions and may reduce the severity of lymphadenitis. Unless treatment is delayed, surgical drainage of the abscess is rarely needed.

Bệnh nhân nếu nghi ngờ mắc bệnh Tularemia sẽ được nhập viện vì các lý do lâm sàng
Tularemia is a dangerous infectious disease that affects both animals and humans. Therefore, the diagnosis, treatment and prevention of this disease should be closely monitored and thoroughly disinfected. Although a person will not get it again after recovering from Tularemia for a long time, a second infection is possible. Therefore, if signs of disease appear, patients need to quickly go to reputable medical facilities to be examined, diagnosed and treated by a specialist.
Vinmec International General Hospital is the address for examination, treatment and prevention of diseases. When performing the examination process at Vinmec, customers will be welcomed and used modern facilities and equipment along with perfect medical services under the guidance and advice of experts. Good doctors, well-trained both at home and abroad.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.