This is an automatically translated article.
The article was professionally consulted by Doctor Trinh Le Hong Minh - Radiologist - Radiology Department - Vinmec Central Park International General Hospital.Superior vena cava syndrome can result from extrinsic compression, intrinsic stenosis, or intraluminal thrombosis. In particular, malignant tumors are often the main cause of superior vena cava occlusion and are considered an oncology emergency. Therefore, if not diagnosed and intervened promptly, superior vena cava occlusion will quickly threaten the patient's life.
1. What is superior vena cava syndrome?
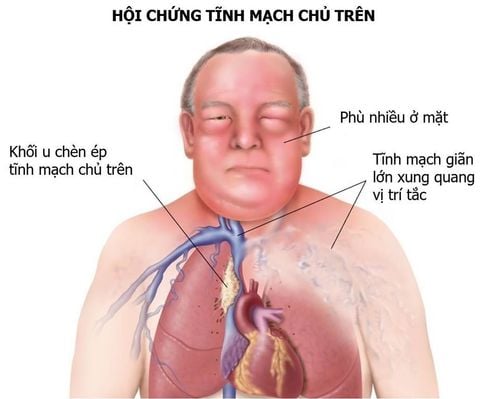
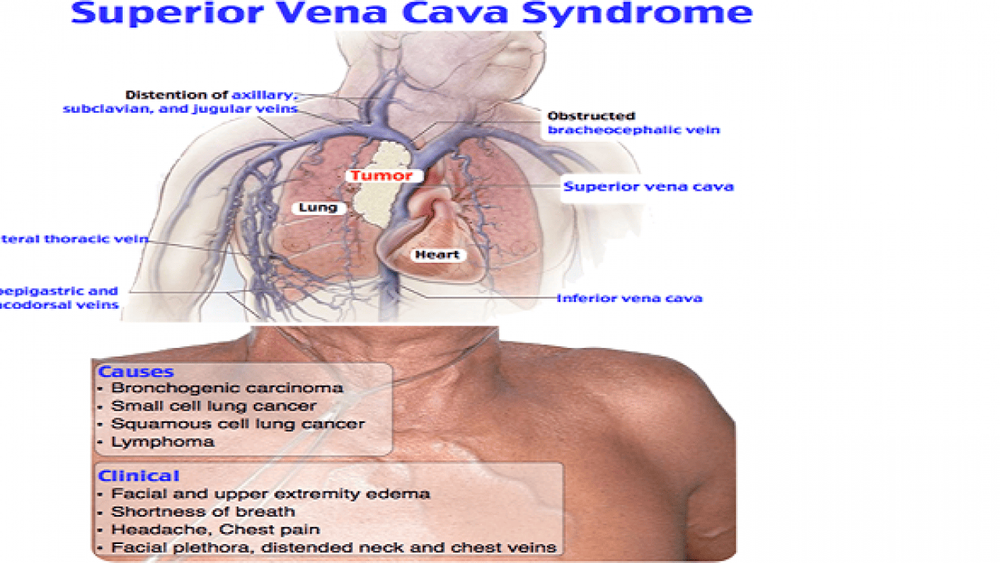
The superior vena cava is the main drainage vessel for venous blood from the head, neck, upper extremities and upper chest to the right atrium. The superior vena cava is located in the mediastinum and is surrounded by relatively rigid structures such as the sternum, trachea, right bronchus, aorta, pulmonary artery, and perioral lymph nodes and air ducts. manage. Due to the thin wall structure and low pressure, the superior vena cava becomes fragile when it is compressed or blocked.
Superior vena cava is a blockage of blood flow through the superior vena cava. This is a medical emergency and usually presents in patients with an intrathoracic malignancy process. Therefore, when a patient is admitted to the hospital with suspicious signs of superior vena cava occlusion, immediate diagnostic evaluation and treatment is warranted.
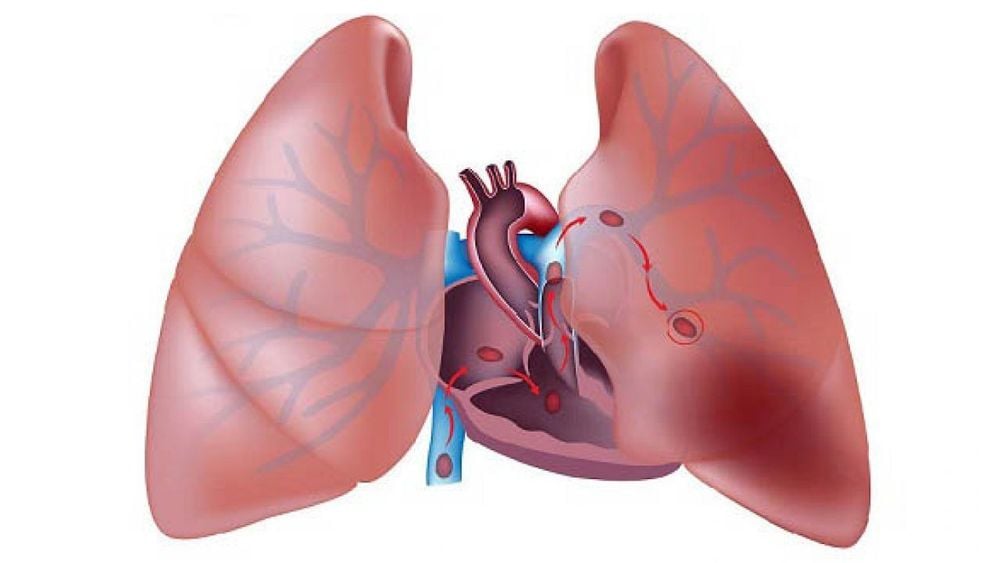
Obstruction of the superior vena cava may be caused by neoplastic invasion of the venous wall associated with intravascular thrombus or simply by external pressure of a tumor on the vena cava above . In particular, for complete superior vena cava obstruction, this is the result of intravascular thrombosis combined with external pressure. In contrast, incomplete superior vena cava obstruction is more often secondary to external pressure without thrombosis.
In addition, nonmalignant conditions can cause superior vena cava occlusion such as mediastinal fibrosis; vascular diseases, such as aortic aneurysms , vasculitis, and arteriosclerosis; infections, such as tuberculosis, syphilis; benign mediastinal tumors such as teratomas, cysts, thymomas and scrotal cysts...
The prognosis in patients with superior vena cava occlusion depends mainly on the course of the underlying disease. If the cause is benign, the patient's life expectancy does not change. In contrast, if secondary to a malignancy, patient survival correlates with tumor histopathology. However, if the patient has complete venous occlusion and has signs and symptoms of laryngeal edema and cerebral edema, life will be rapidly threatened, the risk of sudden death is very high.
2. Approach to clinical diagnosis of superior vena cava occlusion
2.1. Medical history
In the early stages of the clinical course of superior vena cava syndrome, partial obstruction of the superior vena cava may be asymptomatic or often overlooked with vague symptoms.
As the syndrome progresses to total vena cava obstruction, the classic symptoms and signs become more apparent. Specifically, shortness of breath is the most common symptom, other symptoms include facial swelling, headache, cough, arm swelling, chest pain, difficulty swallowing, visual field disturbances, hoarseness, slurred speech, nasal congestion, nausea, pleural effusion, and dizziness.
2.2. Examination
The characteristic physical signs of superior vena cava occlusion include distension of the jugular and thoracic veins, facial edema, upper extremity edema, altered mental status, pleural effusion, cyanosis, papilledema, and stupor. touch and even coma.
Sometimes, symptoms that change with the patient's position such as leaning forward or lying down can aggravate these symptoms.
2.3. Symptoms
Complications of superior vena cava occlusion may include:
Laryngeal edema Cerebral edema Decreased cardiac output with hypotension Pulmonary embolism (when associated thrombosis)
3. Imaging facilities for clinical diagnosis of superior vena cava occlusion
Patients with superior vena cava occlusion syndrome can be diagnosed by physical examination alone. However, convincing evidence still requires diagnostic imaging3.1. Chest X-ray
Chest radiograph may show a dilated mediastinum or a mass on the right side of the chest.
3.2. Computerized tomography
Computed tomography (CT) has the advantage of providing more precise information about the location of the obstruction and can guide biopsies by mediastinoscopy, bronchoscopy or fine needle aspiration through the skin. The tool also provides information about other important structures, such as the bronchi and vocal cords.
Accordingly, compared with conventional x-ray, chest CT is often the initial test of choice to determine whether the obstruction is due to external compression or thrombosis. Additional information is needed because the presence of these structures directs the need for prompt intervention to relieve pressure on the head-face-neck area.

3.3. Magnetic resonance imaging
Magnetic resonance imaging (MRI) has not been fully studied in the context of diagnosing superior vena cava occlusion, but it is also a promising tool. MRI has several potential advantages over CT in that it provides multiple viewing angles, allows direct visualization of blood flow, and does not require iodinated contrast such as CT scans.
Therefore, MRI is an acceptable alternative for patients with renal failure or those with contrast allergy. The potential disadvantages of using an MRI are that it takes more time and is more expensive.
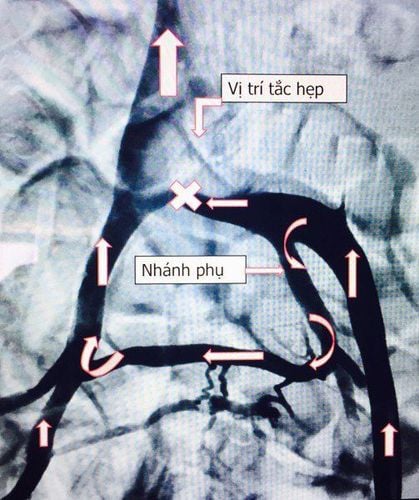
3.4. Venous scan
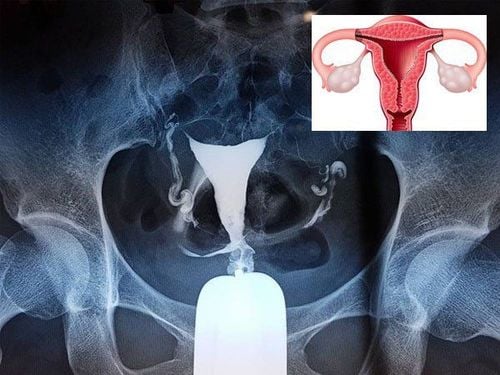
Venography is the most accurate diagnostic tool, especially helping to pinpoint the exact cause of superior vena cava obstruction.
This is especially important if surgical management is being considered for acute vena cava obstruction.
Today, technetium-99m radionuclide angiography is an alternative minimally invasive method for imaging the venous system. Although the images obtained with this method are not as well defined as those obtained with previous contrast angiography, this tool still shows the potency and volume of the flows.
3.5. Other tools
Most patients have superior vena cava occlusion present before an etiological diagnosis is established. Therefore, treatment without a definitive diagnosis should be initiated only in patients with rapidly progressive symptoms or in whom repeated unsuccessful histological attempts have been made.
Fortunately, other relatively non-invasive or semi-invasive measures also help to identify the etiology in the setting of superior vena cava occlusion such as sputum cytology, bronchoscopy...
4. How to treat superior vena cava occlusion?
In the treatment of superior vena cava syndrome, the goal is to relieve symptoms and attempt to cure the primary malignancy. Indeed, only a small percentage of patients with superior vena cava obstruction are rapid-onset and at risk for life-threatening complications.
Patients with a clinical presentation of vena cava occlusion will often experience significant improvement in symptoms from conservative management measures, including elevation of the head of the bed and supplemental oxygen. Emergency treatment is indicated in the presence of cerebral edema, decreased cardiac output, or upper respiratory tract edema. Corticosteroids and diuretics are often used to reduce laryngeal or cerebral edema. At the same time, radiation therapy has also been approved as a standard treatment for most of these patients. In addition, chemotherapy may be preferable to radiation therapy for patients with tumors that are more sensitive to chemotherapy.
Antithrombotic treatments are instituted when superior vena cava occlusion is due to peritubular vena cava thrombosis with thrombolytics (eg, streptokinase, urokinase, or recombinant tissue plasminogen activator) or anticoagulants (eg, heparin or oral anticoagulants). These drugs are most effective when patients are treated within 5 days of the onset of symptoms.
Interventional treatment in superior vena cava occlusion, including percutaneous endovascular stenting, venous angioplasty combined with stenting... need to be carefully consulted with the patient, especially in these situations. situation of advanced cancer and must have consensus of many experts such as thoracic surgery, hematology and oncology.

In summary, superior vena cava syndrome is a collection of clinical signs and symptoms caused by partial or complete obstruction of intravascular blood flow. This obstruction is usually the result of venous thrombus formation or tumor infiltration into the vessel wall, according to the diagnostic means of superior vena cava occlusion. From there, treatment options will be considered, both to improve symptoms and maintain the patient's quality of life.
Currently, Vinmec International General Hospital has been and continues to be fully equipped with modern diagnostic facilities such as: PET/CT, SPECT/CT, MRI... biology, immunohistochemistry, genetic testing, molecular biology testing, as well as a full range of drugs to treat diseases. Accordingly, the process of examination and accurate diagnosis of the disease is carried out by experienced and qualified doctors.
After having an accurate diagnosis of the disease and stage, the patient will be consulted to choose the most appropriate and effective treatment methods. The treatment process is always closely coordinated with many specialties: Diagnostic Imaging, Biochemistry, Immunology, Cardiology, Stem Cell and Gene Technology; Department of Rehabilitation, Department of Psychology, Department of Nutrition... to bring the highest efficiency and comfort to the patient.
Especially, now to improve service quality, Vinmec also deploys many packages of General Health Checkup that can detect diseases early for timely examination and treatment.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference source: emedicine.medscape.com