This is an automatically translated article.
Treatment of obsessive-compulsive disorder may not cure you completely, but it can help control symptoms to increase quality of life. Treatment may include non-drug approaches, psychological support, and the use of certain medications to improve symptoms.
1. Diagnosis of Obsessive Compulsive Disorder (OCD)
Steps to help diagnose obsessive-compulsive disorder may include:
Psychological assessment: Includes discussion of your thoughts, feelings, symptoms, and behavioral patterns to determine if you have Whether an obsession or compulsive behavior affects quality of life. Or, with permission, your doctor can talk to your family or friends. OCD diagnostic criteria. Your doctor may use the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. Physical examination. This is done to help rule out other problems that may be causing your symptoms and to check for any related complications. It is sometimes difficult to diagnose OCD because the symptoms can be similar to those of OCD, anxiety disorders, depression, schizophrenia, or other mental health disorders. another god. You can also have both OCD and another mental health disorder at the same time. Talk to your doctor so that they can be properly diagnosed and treated.
2. Treatment of Obsessive Compulsive Disorder
Treatment for obsessive-compulsive disorder may not cure it, but it can help control symptoms so they don't dominate your daily life. Depending on the severity of OCD, some people may need long-term, ongoing, or more intensive treatment.
The two main treatments for OCD are psychotherapy and medication. Often, the most effective treatment is a combination of these methods.
2.1. Psychotherapy
Cognitive behavioral therapy (CBT), a type of psychotherapy, is effective for many people with OCD. Exposure and response prevention (ERP), a component of CBT therapy, is that you are gradually exposed to the feared object or phobia, such as dirt, and you must learn to resist the withdrawal. enforce their coercive “rituals”. ERP needs effort and drastic action. As difficult as it may be, the result is that you can enjoy a better quality of life when you learn to manage your obsessions and compulsions.
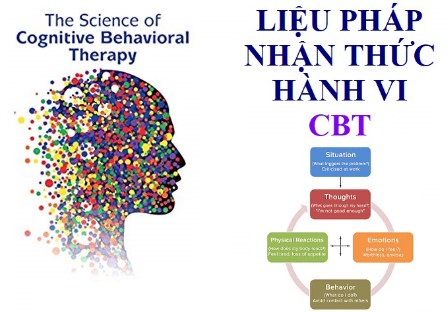
Liệu pháp nhận thức hành vi là một phương pháp điều trị rối loạn ám ảnh cưỡng chế.
2.2. Drug treatment
Certain psychiatric medications can help control OCD's obsessions and compulsions. Usually, antidepressants are tried first.
Antidepressants approved by the Food and Drug Administration (FDA) to treat OCD include:
Clomipramine (Anafranil) for adults and children 10 years of age and older. Fluoxetine (Prozac) is for adults and children 7 years of age and older. Fluvoxamine for adults and children 8 years of age and older. Paroxetine (Paxil, Pexeva) is for adults only. Sertraline (Zoloft) is for adults and children 6 years of age and older. However, your doctor may prescribe antidepressants and other psychiatric medications.
Here are some things to discuss with your doctor about OCD medications:
Choosing an appropriate medication. In general, the goal is effective control of symptoms at the lowest possible dose. It's not uncommon for you to try multiple medications before you find the one that works best. Your doctor may recommend a variety of medications to effectively control your symptoms. It may take weeks to months after you start taking the medicine for you to notice an improvement in your symptoms. Side Effects. All psychiatric medications have potential side effects. Talk to your doctor about possible side effects and the need to monitor your health while taking psychiatric medications. Tell your doctor if you experience worrisome side effects. Suicide risk. Most antidepressants are generally safe, but the FDA requires all antidepressants to have a "black box warning," the strictest warning against prescriptions. In some cases, children, adolescents, and young adults under 25 years of age may experience an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when changing dose change. If you are thinking about suicide, contact your doctor right away or get emergency help. Remember, antidepressants are more likely to reduce the risk of suicide in the long run by improving mood. Interaction with other substances. When taking antidepressants, tell your doctor about any prescription or over-the-counter medications, herbs, or supplements you're taking. Some antidepressants can make others less effective and cause dangerous reactions when combined with them. Stop taking antidepressants. Antidepressants are not considered addictive, but sometimes physical dependence (which is different from addiction) can occur. So stopping treatment suddenly or missing a few doses can cause withdrawal-like symptoms, sometimes called discontinuation syndrome. Don't stop taking your medication without consulting your doctor, even if you're feeling better, you could have a relapse of your OCD symptoms. Follow your doctor's instructions for a gradual and safe dose reduction. Talk to your doctor about the risks and benefits of using specific medications.
2.3. Other methods of treatment
Sometimes psychotherapy and medications are not effective enough to control OCD symptoms. In treatment-resistant cases, other options may be offered such as:
Intensive inpatient and outpatient programs. Comprehensive treatment programs that focus on the principles of ERP therapy can be helpful for people with OCD who are struggling with the ability to function due to the severity of their symptoms. These programs will usually last several weeks. Deep brain stimulation (DBS). DBS is FDA-approved to treat OCD in adults 18 years of age and older who have not responded to traditional treatments. DBS involves implanting electrodes into certain regions of your brain. These electrodes generate electrical pulses that can help correct abnormal pulses. Transcranial magnetic stimulation (TMS). The FDA has approved a specific device (BrainsWay Deep Transcranial Magnetic Stimulation) to treat OCD in adults aged 22 to 68 years when traditional treatments have not worked. TMS is a non-invasive procedure that uses a magnetic field to stimulate nerve cells in the brain to improve symptoms of OCD. During a TMS session, an electromagnetic coil is placed into the scalp near your forehead. Electromagnets deliver a magnetic pulse that stimulates nerve cells in your brain.
3. Lifestyle adjustments and home remedies
Obsessive-compulsive disorder is a chronic condition, which means it may never go away. Although you treat OCD with a doctor's supervision, there are a few things you can do yourself to develop your treatment plan:
Practice what you learn. Work with your psychiatrist to identify techniques and skills that help manage symptoms and practice them regularly. Take medication as directed. Even if you are feeling well, do not stop taking your medicine suddenly. If you stop, OCD symptoms are likely to return. Pay attention to warning signs. You and your doctor may have identified problems that may be causing OCD symptoms. Make a plan to know what to do if symptoms return. Contact your doctor or therapist if you notice any changes in your symptoms or sensations. Check before taking other medications. Contact the doctor who is treating you for OCD before you take medication prescribed by another doctor or before taking any over-the-counter medications, vitamins, herbs, or other supplements to avoid interactions. can happen.

Rối loạn ám ảnh cưỡng chế cần điều trị bằng cách uống thuốc theo chỉ dẫn của bác sĩ.
4. Facing OCD and its methods of support
Coping with obsessive-compulsive disorder can be challenging. Medicines can have unwanted side effects, and you may feel embarrassed or angry when you have a condition that requires long-term treatment. Here are some ways to help cope with OCD:
Learn about OCD. Learning about your condition can energize you and motivate you to stick with your treatment plan. Focus on your goal. Keep your recovery goals in mind and remember that recovery from OCD is an ongoing process. Join a support group. Reaching out to others who are also facing similar challenges can provide you with support and help you cope with the challenges. Do healthy things. Explore healthy ways that can energize you, such as recreational activities, regular exercise, healthy eating, and adequate sleep. Learn relaxation and stress management. In addition to professional treatment, stress management techniques such as meditation, visualization, muscle relaxation, massage, deep breathing, yoga, or tai chi can help reduce stress and anxiety. Stick with your daily activities. Try not to avoid meaningful activities. Go to work or school as you normally would. Spend time with family and friends. Don't let OCD get in the way of your life.
5. Prepare for doctor visits
Because obsessive-compulsive disorder often requires special care, you may be referred to a mental health professional, such as a psychiatrist or psychologist, for evaluation and treatment. treat.
To prepare for your appointment, think about your treatment needs and goals. Make a list of:
Any symptoms you notice, including the types of obsessions and compulsions you've experienced and things you may be avoiding because you're too worried. Any major stressors, recent life changes, and similar symptoms (if any) in your family members. All medications, vitamins, herbal remedies or other supplements you are currently taking and the dosage. Questions to ask your doctor or therapist.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.
Reference article: mayoclinic.org