This is an automatically translated article.
Article by Master, Doctor Nguyen Ngoc Phu - Department of Intensive Care - Vinmec Times City International Hospital
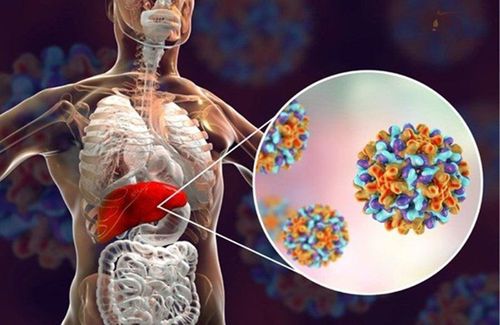
Hepatic encephalopathy is a decline in brain function that occurs as a result of severe liver disease. In this condition, your liver cannot completely remove toxins from the blood. This causes a build-up of toxic products in your blood, which can lead to brain damage.
Hepatic encephalopathy can be acute or chronic. In some cases, a person with hepatic encephalopathy can become unresponsive and fall into a coma.
1. What are the common types of hepatic encephalopathy?
Acute hepatic encephalopathy occurs due to advanced liver disease. This mainly happens in people with the following conditions:
Acute fulminant hepatitis : This is a type of severe viral hepatitis that comes on suddenly. Toxic hepatitis: Toxic hepatitis can be caused by exposure to alcohol, chemicals, drugs or certain dietary supplements. Reye's syndrome: This is a particularly severe acute liver injury and brain edema. Seen mainly in children. Acute hepatic encephalopathy can also be a sign of end-stage liver failure.
People with chronic hepatic encephalopathy may have permanent or recurrent episodes. They need ongoing treatment to help prevent symptoms from getting worse. Recurrent cases are often seen in people with severe cirrhosis. Cases of permanent hepatic encephalopathy are rare and occur in people who do not respond to treatment and who have permanent neurological conditions such as seizures and spinal cord injuries.
2. What are the clinical symptoms of hepatic encephalopathy?
Depending on the cause and severity, people with hepatic encephalopathy will have different clinical manifestations.
Symptoms and signs of moderate hepatic encephalopathy may include:
Difficulty thinking Mood changes Decreased concentration Hand tremors, trouble writing Confusion, anxiety Frequent forgetting Difficulty commenting on problems Bad breath Symptoms of severe hepatic encephalopathy are:
Confusion Somnolence or coma Anxiety, fear Convulsions Severe mood changes Fatigue Chatter, confusion Hand tremors Slow movements Patient You will need immediate medical attention and treatment if symptoms develop. These symptoms can lead to coma if the person is not treated quickly.

Hội chứng não gan có thể gây triệu chứng run tay
3. What causes hepatic encephalopathy?
The exact cause of hepatic encephalopathy remains unknown. However, the trigger is usually due to the accumulation of toxins in the blood. This happens when your liver is no longer able to completely break down toxins.
Your liver removes harmful chemicals like ammonia from your body. These toxins are left over when proteins are metabolized or broken down for use by different organs in your body. Your kidneys convert these toxins into safer substances, which are then eliminated from your body in your urine.
When your liver is damaged, it cannot filter all the toxins. The toxins can then build up in your bloodstream and potentially enter your brain. Toxic buildup can also damage other organs and nerves.
Factors that can trigger hepatic encephalopathy:
Infection: pneumonia Kidney damage, pathology Dehydration Lack of oxygen or low oxygen levels Recent surgery or injury Medicines that suppress the immune system Overeating Protein Central nervous system depressants such as barbiturates or benzodiazepines Electrolyte disturbances, especially hypokalemia following vomiting or diuretic use.
4. How is hepatic encephalopathy diagnosed?
There are several tests used to diagnose hepatic encephalopathy.
4.1. Blood tests A complete blood count: Checks for red blood cells, white blood cells, and platelets in your blood. A low red blood cell count indicates anemia and will lead to tissue hypoxia.
Blood tests can also be used to measure the levels of sodium, potassium, and ammonia in your blood. Elevated levels of these substances are a sign of impaired liver function.
4.2. Imaging Diagnostic imaging tests, such as computed tomography or nuclear magnetic resonance imaging, can help check for bleeding in your brain or abnormalities in your brain.
4.3. Liver function tests Liver function tests: measure the activity of enzymes such as GOT, GPT, GGT, total bilirubin, direct bilirubin... If there is an increase in these substances, it indicates a decline in function. liver or destroy your liver cells.
Telling your doctor a history of liver disease, if any, of kidney disease, along with the symptoms you are experiencing can sometimes be enough to help your doctor diagnose hepatic encephalopathy.

Xét nghiệm chức năng gan giúp chẩn đoán hội chứng não gan
5. What are the different stages of hepatic encephalopathy?
Based on the severity of symptoms, hepatic encephalopathy is divided into stages. Common grading systems include: West Haven criterion and Glasgow scale.
The five stages of hepatic encephalopathy, according to West Haven criteria are:
Stage 0 – Change in personality or behavior. Changes in memory, concentration, intellectual function, and coordination. There is no Asterixis.
Stage 1 – Negligible lack of awareness. Shorten attention span. Hypersomnia, insomnia, reversal of sleep patterns. Depression, discomfort. There may be Asterixis.
Stage 2 – Apathy or apathy. Disorientation. Disrespectful in behavior. Asterixis is evident. Drowsiness, lethargy, obvious personality changes, inappropriate behavior, and persistent disorientation, usually over time.
Stage 3 – Dozed off but may be aroused, disorientation to time and place, confusion, memory loss, frequent anger, inability to understand speech
Stage 4 – Coma or no response to painful stimuli
6. What is the treatment for hepatic encephalopathy?
Treatment options for hepatic encephalopathy depend on the severity and underlying cause of the condition.
You may need to eat less protein if the condition is caused by eating too much protein. Because protein is needed for your body to function properly, a dietitian or doctor can develop a diet that allows you to get enough protein without making your symptoms worse. High protein foods to avoid include: Poultry, red meat, eggs, shrimp, crab, fish...
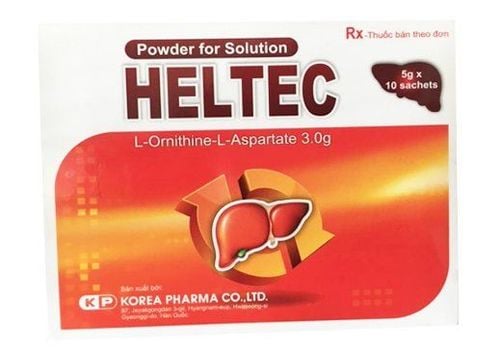
Medicines can also help slow the rate at which toxins are absorbed into the bloodstream. Your doctor may prescribe antibiotics (metronidazole) and the sugar lactulose (duphalac), a synthetic sugar. These drugs can help diffuse ammonia (NH3) from the bloodstream into the intestines, and on the one hand destroy the intestinal bacteria that produce NH3. Ammonia in the intestines is converted to a non-diffusing ammonium salt (NH4), which is then eliminated by your body in the stool.
In severe cases causing difficulty breathing, a ventilator or an oxygen mask may be needed.
Some people with this condition may need a liver transplant if eligible.
7. What is the long-term strategy for hepatic encephalopathy?
People with chronic hepatic encephalopathy have better recovery rates than those with acute form. Recovery rates increase if you get treatment early, before your condition gets worse.
With appropriate treatment, hepatic encephalopathy and symptoms can be reversed.
8. What are the complications associated with hepatic encephalopathy?
Complications that may be irreversible include:
Organ failure Cerebral edema Brain herniation

Hội chứng não gan gây chứng liên quan đến bệnh não như phù não
9. How to manage and prevent hepatic encephalopathy?
Treatment, management and prevention of liver disease is the best way to prevent hepatic encephalopathy. You can reduce your risk of liver disease by taking the following steps:
Avoid alcohol or drink less alcohol (as recommended). Avoid high-fat foods. Maintain a healthy weight. Do not share contaminated needles. To avoid viral hepatitis:
Wash your hands thoroughly after using the toilet or changing diapers. Do not share contaminated needles. Avoid close contact with people diagnosed with viral hepatitis. Vaccination against hepatitis A, B. Liver encephalopathy, if detected early and eliminating risk factors such as gastrointestinal bleeding, hypokalemia, etc., will help patients have a better prognosis.
Vinmec International General Hospital is the leading prestigious hospital in the diagnosis and treatment of liver diseases. Patients will be examined and diagnosed with the most modern methods today, with the support of high-tech machines for accurate results.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and to manage your bookings easily.